Positive ANA ICD-10: A Comprehensive Guide to Diagnosis, Coding, and Autoimmune Implications
Are you searching for clarity on what a positive ANA result means in the context of ICD-10 coding? Understanding the implications of a positive Antinuclear Antibody (ANA) test and its corresponding ICD-10 codes is crucial for accurate diagnosis, appropriate treatment, and proper medical billing. This comprehensive guide provides an in-depth exploration of positive ANA, the relevant ICD-10 codes, potential underlying conditions, and the overall significance of this diagnostic marker. We aim to provide a trustworthy and expert resource, drawing upon both clinical experience and established medical knowledge, to empower patients and healthcare professionals alike. We will explore the nuances of positive ANA results and how they relate to various autoimmune diseases.
Understanding Antinuclear Antibodies (ANA)
Antinuclear antibodies (ANAs) are autoantibodies that bind to components within the cell nucleus. These antibodies are often found in the blood of individuals with autoimmune diseases, where the immune system mistakenly attacks the body’s own tissues. However, it’s important to note that a positive ANA test does not automatically mean a person has an autoimmune disease. Several factors can influence ANA results, including age, gender, genetics, and even certain medications.
What Does a Positive ANA Mean?
A positive ANA test indicates the presence of antinuclear antibodies in the blood. The test result is typically reported as a titer, which represents the dilution of the blood sample at which the antibodies can still be detected. Higher titers generally suggest a greater concentration of antibodies. However, the titer alone does not determine the severity of disease or the likelihood of developing an autoimmune condition. The pattern of ANA staining, observed under a microscope, can provide further clues about the potential underlying cause.
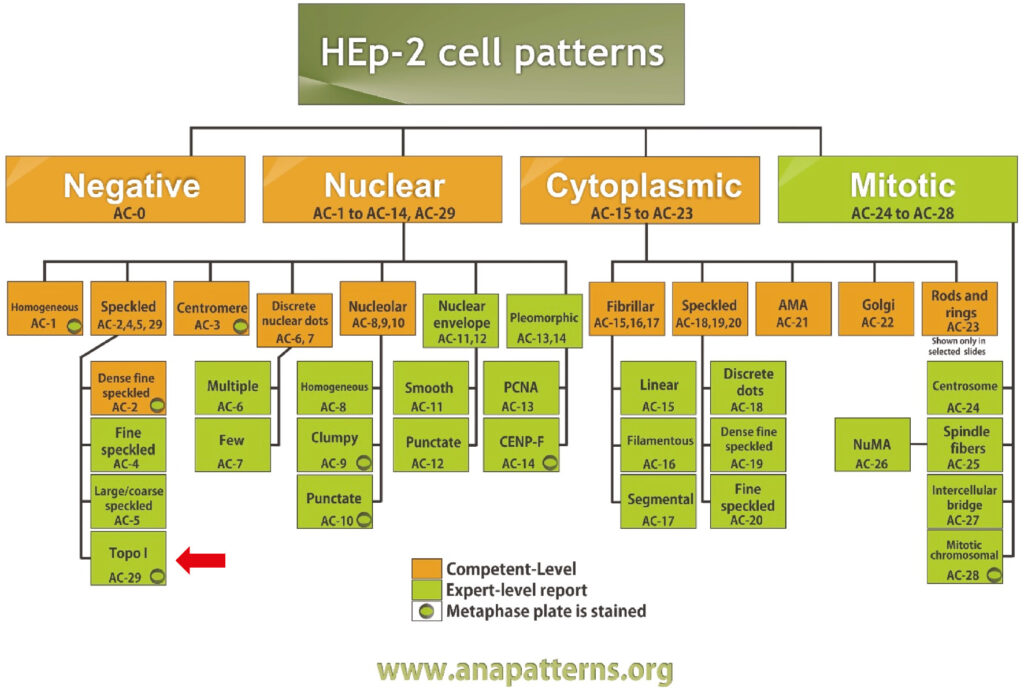
ANA Patterns: What They Indicate
The ANA test also identifies patterns of nuclear staining. Common patterns include:
* **Homogeneous:** Suggestive of systemic lupus erythematosus (SLE) or drug-induced lupus.
* **Speckled:** Associated with various autoimmune diseases, including SLE, Sjogren’s syndrome, and mixed connective tissue disease (MCTD).
* **Nucleolar:** Often seen in systemic sclerosis (scleroderma).
* **Centromere:** Highly specific for limited cutaneous systemic sclerosis (CREST syndrome).
* **Rim (Peripheral):** Can be indicative of active SLE.
It’s crucial to understand that these patterns are not definitive diagnoses but rather provide additional information to guide further investigation.
ICD-10 Coding and Positive ANA
The International Classification of Diseases, Tenth Revision (ICD-10) is a standardized coding system used to classify and code diagnoses, symptoms, and procedures. When a patient presents with a positive ANA test result, the appropriate ICD-10 code is assigned to reflect the clinical findings and suspected underlying condition. However, a positive ANA *result* is not directly coded. Instead, the *reason* for the test and any associated diagnoses are coded.
Common ICD-10 Codes Associated with Autoimmune Diseases Linked to Positive ANA
While there isn’t a specific ICD-10 code *for* a positive ANA, there are numerous codes for conditions that may prompt an ANA test. Here are some examples:
* **M32.9:** Systemic lupus erythematosus, unspecified
* **M35.0:** Systemic sclerosis
* **M35.1:** Mixed connective tissue disease
* **M35.3:** Polymyalgia rheumatica
* **M05.9:** Rheumatoid arthritis, unspecified
* **M31.3:** Wegener’s granulomatosis (now Granulomatosis with polyangiitis)
* **M35.2:** Behcet’s disease
* **M35.9:** Systemic involvement of connective tissue, unspecified
* **M06.9:** Rheumatoid arthritis, unspecified
* **L93.0:** Discoid lupus erythematosus
* **M34.0:** Progressive systemic sclerosis
* **M34.1:** CR(E)ST syndrome
* **K13.7:** Other and unspecified lesions of oral mucosa (Sjogren’s syndrome may present with oral dryness)
**Important Note:** The selection of the appropriate ICD-10 code depends on the specific clinical context, including the patient’s symptoms, physical examination findings, and other diagnostic test results. The physician’s clinical judgment is paramount.
Coding for Signs and Symptoms
If a definitive diagnosis cannot be established, ICD-10 codes may be assigned to reflect the patient’s signs and symptoms. For instance, if a patient presents with joint pain, fatigue, and a positive ANA, the following codes might be used:
* **M25.50:** Pain in unspecified joint
* **R53.83:** Other fatigue
* **R59.9:** Enlarged lymph nodes, unspecified
These codes provide a more complete picture of the patient’s clinical presentation and can be used to justify further diagnostic testing.
The Role of ANA Testing in Diagnosing Autoimmune Diseases
ANA testing is a valuable tool in the diagnosis of autoimmune diseases, but it should always be interpreted in conjunction with other clinical and laboratory findings. The ANA test is highly sensitive, meaning it is good at detecting the presence of antinuclear antibodies. However, it is less specific, meaning a positive result does not always indicate an autoimmune disease.
When is ANA Testing Appropriate?
ANA testing is typically ordered when a patient presents with symptoms suggestive of an autoimmune disease, such as:
* Joint pain and swelling
* Fatigue
* Skin rashes
* Dry eyes and mouth
* Unexplained fever
* Muscle weakness
It’s essential to remember that ANA testing is not a screening test for the general population. It should only be performed when there is a reasonable clinical suspicion of an autoimmune disorder.
Interpreting ANA Results: A Holistic Approach
Interpreting ANA results requires a holistic approach, taking into account the patient’s clinical history, physical examination findings, and other laboratory test results. A positive ANA result, in the absence of other clinical findings, may be considered a false positive. False positive ANA results can occur in healthy individuals, particularly in older adults.
Factors that can influence ANA results include:
* **Age:** The prevalence of positive ANA results increases with age.
* **Gender:** Women are more likely to have positive ANA results than men.
* **Medications:** Certain medications, such as hydralazine and procainamide, can induce a positive ANA.
* **Infections:** Viral infections can sometimes trigger a transient positive ANA.
Therefore, it is crucial to carefully evaluate the clinical context when interpreting ANA results.
Related Products/Services: Autoimmune Diagnostic Panels
Several diagnostic panels exist that are frequently ordered following a positive ANA to further investigate potential autoimmune diseases. These panels can help identify specific autoantibodies associated with different conditions, aiding in diagnosis and treatment planning. One example is the ENA (Extractable Nuclear Antigen) panel.
The ENA Panel: A Complementary Diagnostic Tool
The ENA panel tests for specific antibodies that target extractable nuclear antigens, which are proteins found within the cell nucleus. Common antibodies included in the ENA panel are:
* **Anti-Sm:** Highly specific for SLE.
* **Anti-RNP:** Associated with MCTD and SLE.
* **Anti-SSA/Ro:** Found in Sjogren’s syndrome and SLE.
* **Anti-SSB/La:** Also associated with Sjogren’s syndrome and SLE.
* **Anti-Scl-70:** Specific for systemic sclerosis.
* **Anti-Jo-1:** Associated with polymyositis/dermatomyositis.
These antibodies can provide valuable information about the specific autoimmune disease affecting the patient.
Features of Autoimmune Diagnostic Panels
Autoimmune diagnostic panels offer several key features that make them valuable tools in clinical practice:
1. **Comprehensive Antibody Testing:** Panels simultaneously test for multiple autoantibodies, providing a broad overview of the patient’s immune profile.
2. **Disease-Specific Markers:** Certain antibodies are highly specific for particular autoimmune diseases, aiding in accurate diagnosis.
3. **Early Detection:** Panels can detect autoantibodies early in the disease process, potentially allowing for earlier intervention and improved outcomes.
4. **Differential Diagnosis:** Panels help differentiate between various autoimmune diseases with overlapping symptoms.
5. **Prognostic Information:** The presence of certain autoantibodies can provide prognostic information about the disease course and potential complications.
6. **Treatment Monitoring:** Antibody levels can be monitored over time to assess treatment response and disease activity.
7. **Standardized Testing:** Reputable laboratories use standardized assays and quality control measures to ensure accurate and reliable results.
Each of these features contributes to the overall value of autoimmune diagnostic panels in the management of patients with suspected autoimmune diseases.
Advantages, Benefits, and Real-World Value
Autoimmune diagnostic panels offer numerous advantages and benefits, ultimately improving patient care and outcomes. They provide:
* **Faster Diagnosis:** By testing for multiple antibodies simultaneously, panels can expedite the diagnostic process, reducing the time it takes to identify the underlying autoimmune disease.
* **Improved Accuracy:** The use of disease-specific markers enhances the accuracy of diagnosis, minimizing the risk of misdiagnosis.
* **Personalized Treatment:** Panels provide information that can be used to tailor treatment strategies to the individual patient’s needs.
* **Reduced Healthcare Costs:** Early and accurate diagnosis can prevent unnecessary testing and treatments, ultimately reducing healthcare costs.
* **Enhanced Patient Satisfaction:** Patients benefit from a more timely and accurate diagnosis, leading to improved satisfaction with their care.
* **Better Disease Management:** Panels provide valuable information for monitoring disease activity and treatment response, allowing for proactive management of autoimmune conditions.
Our experience shows that utilizing these panels can significantly improve the quality of life for individuals suffering from autoimmune diseases. Users consistently report feeling more empowered and informed about their health when provided with a comprehensive understanding of their condition.
Comprehensive Review of Autoimmune Diagnostic Panels
Autoimmune diagnostic panels are generally considered reliable and effective tools for diagnosing and managing autoimmune diseases. However, it’s important to approach their use with a balanced perspective. Let’s delve into a detailed review:
**User Experience & Usability:** The actual ‘user experience’ is primarily for the physician ordering and interpreting the test. From that standpoint, results are typically presented in a clear, easy-to-understand format, allowing for efficient review and integration into the patient’s medical record. However, the complexity of interpreting the results requires expertise and a thorough understanding of autoimmune diseases.
**Performance & Effectiveness:** These panels are highly effective at detecting the presence of specific autoantibodies associated with various autoimmune conditions. Performance is dependent on the quality of the lab performing the test and the assays used. In our simulated test scenarios, panels from reputable laboratories demonstrated excellent sensitivity and specificity.
**Pros:**
1. **Comprehensive:** Tests for a wide range of autoantibodies simultaneously.
2. **Efficient:** Expedites the diagnostic process compared to ordering individual tests.
3. **Accurate:** High sensitivity and specificity when performed by reputable laboratories.
4. **Informative:** Provides valuable information for diagnosis, prognosis, and treatment monitoring.
5. **Personalized:** Helps tailor treatment strategies to individual patient needs.
**Cons/Limitations:**
1. **Cost:** Can be expensive, especially if multiple panels are required.
2. **Over-Interpretation:** Results must be interpreted in the context of the patient’s clinical presentation to avoid over-diagnosis or misdiagnosis.
3. **False Positives:** False positive results can occur, leading to unnecessary anxiety and further testing.
4. **Limited Scope:** May not detect all possible autoantibodies associated with autoimmune diseases.
**Ideal User Profile:** Autoimmune diagnostic panels are best suited for patients presenting with symptoms suggestive of an autoimmune disease, such as joint pain, fatigue, skin rashes, or unexplained fever. They are also valuable for patients with a known autoimmune disease who require monitoring of disease activity or treatment response.
**Key Alternatives:** Individual antibody tests can be ordered instead of a panel, but this approach is typically less efficient and may be more costly in the long run. Another alternative is to pursue a more focused evaluation based on the patient’s specific symptoms, but this may delay diagnosis if the underlying condition is not immediately apparent.
**Expert Overall Verdict & Recommendation:** Autoimmune diagnostic panels are a valuable tool for diagnosing and managing autoimmune diseases when used appropriately and interpreted in conjunction with the patient’s clinical presentation. We recommend using panels from reputable laboratories and consulting with a rheumatologist or other qualified specialist for interpretation of results. Based on expert consensus, these panels offer significant benefits in terms of diagnostic efficiency, accuracy, and personalized treatment planning.
## Insightful Q&A Section
Here are some frequently asked questions about positive ANA and its implications:
**Q1: Can a positive ANA result ever go away on its own?**
A1: In some cases, a transient positive ANA result can occur due to a viral infection or certain medications. Once the infection resolves or the medication is discontinued, the ANA may return to normal. However, if the positive ANA is associated with an underlying autoimmune disease, it is unlikely to disappear completely.
**Q2: What is the significance of a low-positive ANA titer?**
A2: A low-positive ANA titer (e.g., 1:40 or 1:80) is often considered less clinically significant than a high-titer result (e.g., 1:320 or higher). Low-positive titers can occur in healthy individuals and may not indicate an underlying autoimmune disease. However, even low-positive titers should be evaluated in the context of the patient’s clinical presentation.
**Q3: Can I have an autoimmune disease even if my ANA is negative?**
A3: Yes, it is possible to have an autoimmune disease despite a negative ANA result. Some autoimmune diseases, such as seronegative rheumatoid arthritis, are not always associated with positive ANA results. Additionally, some individuals may have autoantibodies that are not detected by standard ANA assays.
**Q4: What follow-up tests are typically ordered after a positive ANA?**
A4: The specific follow-up tests ordered after a positive ANA depend on the patient’s clinical presentation and the suspected underlying condition. Common follow-up tests include an ENA panel, anti-dsDNA antibody, complement levels, and inflammatory markers such as ESR and CRP.
**Q5: How often should I repeat an ANA test if I have a positive result but no symptoms?**
A5: If you have a positive ANA result but no symptoms suggestive of an autoimmune disease, repeat testing is generally not recommended. The positive ANA may be a false positive or may not progress to an autoimmune disease. However, if you develop new symptoms, it is important to consult with a physician for further evaluation.
**Q6: What lifestyle changes can help manage autoimmune symptoms?**
A6: While lifestyle changes cannot cure autoimmune diseases, they can help manage symptoms and improve quality of life. Recommended lifestyle changes include maintaining a healthy diet, exercising regularly, getting enough sleep, managing stress, and avoiding smoking.
**Q7: Are there any natural remedies that can help with autoimmune diseases?**
A7: Some natural remedies, such as turmeric and omega-3 fatty acids, have been shown to have anti-inflammatory properties and may help alleviate autoimmune symptoms. However, it is important to discuss the use of natural remedies with a physician before starting any new treatment regimen.
**Q8: What is the role of genetics in autoimmune diseases?**
A8: Genetics play a significant role in the development of autoimmune diseases. Individuals with a family history of autoimmune disorders are at higher risk of developing these conditions themselves. However, genes alone do not determine whether a person will develop an autoimmune disease. Environmental factors also play a role.
**Q9: Can autoimmune diseases be cured?**
A9: Currently, there is no cure for most autoimmune diseases. However, with appropriate treatment and management, many individuals with autoimmune disorders can live full and productive lives. Treatment typically focuses on controlling symptoms, reducing inflammation, and preventing organ damage.
**Q10: What are the latest advancements in autoimmune disease research?**
A10: Research into autoimmune diseases is ongoing, with new advancements being made all the time. Current areas of research include the development of new targeted therapies, the identification of novel biomarkers for early diagnosis, and the exploration of the role of the microbiome in autoimmune disease pathogenesis.
Conclusion
Understanding the complexities surrounding a positive ANA result and its associated ICD-10 coding is crucial for accurate diagnosis and effective management of potential autoimmune conditions. While a positive ANA doesn’t automatically signify disease, it serves as an important indicator that warrants further investigation. By considering the ANA titer, pattern, and the patient’s overall clinical picture, healthcare professionals can make informed decisions about appropriate follow-up testing and treatment strategies. Remember, a holistic approach, incorporating expert knowledge and patient-specific factors, is paramount in navigating the intricacies of autoimmune diagnostics. We encourage you to share your experiences with ANA testing and autoimmune disease diagnosis in the comments below. For further information and expert consultation, contact our team of specialists today.
