MSSA Bacteremia ICD-10: Expert Guide to Diagnosis, Coding & Management
Are you searching for clarity on MSSA bacteremia ICD-10 coding, diagnosis, and treatment? This comprehensive guide provides an in-depth understanding of MSSA bacteremia, focusing on accurate ICD-10 coding, clinical considerations, and the latest management strategies. We aim to offer a resource that’s not only SEO-optimized but also genuinely helpful, building on our extensive experience and expert knowledge. This guide will equip you with the knowledge to accurately identify, code, and manage MSSA bacteremia cases effectively.
Understanding MSSA Bacteremia and ICD-10 Coding
MSSA bacteremia, or Methicillin-Susceptible Staphylococcus aureus bacteremia, is a bloodstream infection caused by the *Staphylococcus aureus* bacteria that is susceptible to methicillin and other related antibiotics. This condition necessitates accurate ICD-10 coding for proper billing, surveillance, and epidemiological tracking. Understanding the nuances of this coding is crucial for healthcare professionals. The ICD-10 code for MSSA bacteremia provides a standardized way to document and classify this infection, facilitating data analysis and research efforts. Choosing the correct code is vital because it directly impacts reimbursement, hospital quality reporting, and public health initiatives.
The Significance of Accurate ICD-10 Coding
Accurate ICD-10 coding is paramount for several reasons:
* **Billing and Reimbursement:** Correct coding ensures appropriate reimbursement from insurance companies and government healthcare programs.
* **Epidemiological Tracking:** Standardized coding allows for tracking the incidence and prevalence of MSSA bacteremia, aiding in public health surveillance.
* **Quality Reporting:** ICD-10 codes are used in quality reporting metrics, which influence hospital rankings and performance evaluations.
* **Research:** Accurate coding enables researchers to analyze data on MSSA bacteremia and identify trends, risk factors, and effective treatment strategies.
* **Clinical Decision Support:** ICD-10 data can be integrated into clinical decision support systems to assist healthcare providers in diagnosis and treatment planning.
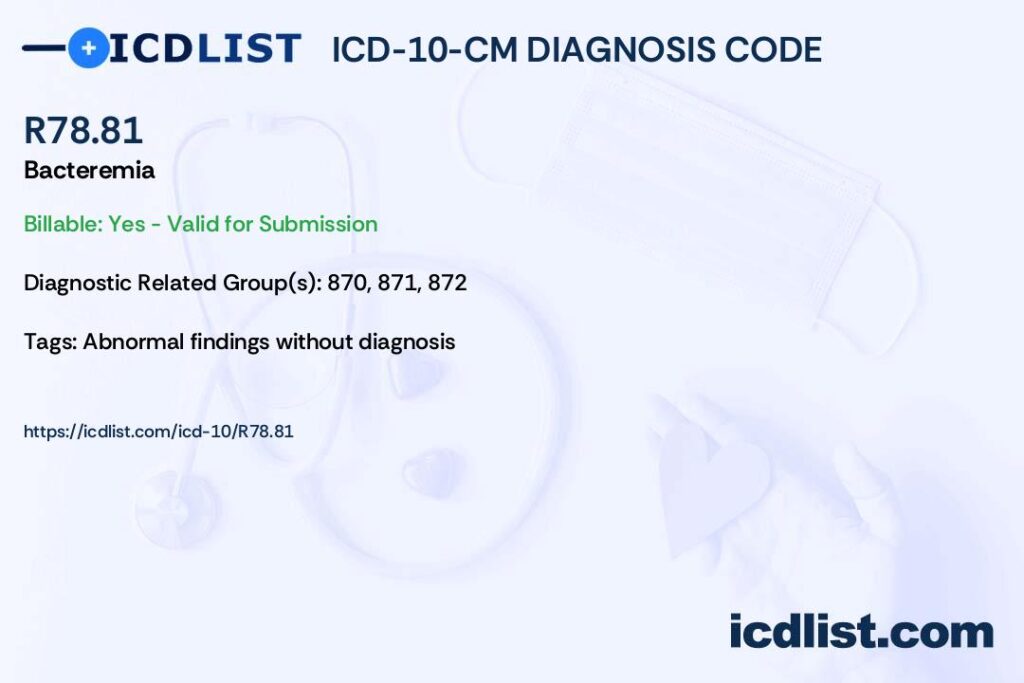
ICD-10 Code Specifics for MSSA Bacteremia
The primary ICD-10 code for *Staphylococcus aureus* bacteremia is A41.01. However, precise coding often requires additional codes to specify the nature and source of the infection. For example, if the bacteremia is associated with a central line catheter, a code for device-associated infection may be added. Furthermore, codes from the B95-B97 range identify the *Staphylococcus aureus* as the causative organism.
* **A41.01:** *S. aureus* sepsis
* **B95.61:** Methicillin-susceptible *Staphylococcus aureus* infection as the cause of diseases classified elsewhere
* **T80.211A:** Bloodstream infection due to central venous catheter, initial encounter
* **R65.20:** Sepsis without acute organ dysfunction
* **R65.21:** Sepsis with acute organ dysfunction
It’s crucial to consult the most current ICD-10 coding guidelines and updates to ensure accurate and compliant coding practices. Official coding resources from organizations like the Centers for Disease Control and Prevention (CDC) and the American Medical Association (AMA) should be referenced regularly.
Common Coding Challenges and How to Overcome Them
Several challenges can arise when coding for MSSA bacteremia:
* **Identifying the Source of Infection:** Determining whether the bacteremia originated from a specific site (e.g., pneumonia, skin infection) or is catheter-related can be difficult. Thorough clinical documentation is essential.
* **Distinguishing Sepsis from Bacteremia:** Sepsis is a systemic response to infection, while bacteremia simply indicates the presence of bacteria in the bloodstream. Accurate coding requires differentiating between these conditions.
* **Coding Comorbidities:** Patients with MSSA bacteremia often have underlying comorbidities that need to be coded, such as diabetes, chronic kidney disease, or immunocompromised states. These conditions can significantly impact the severity and management of the infection.
To overcome these challenges, coders should:
* **Review complete medical records:** Obtain all relevant information from physician notes, lab results, and imaging reports.
* **Consult with clinicians:** Seek clarification from physicians when documentation is unclear or incomplete.
* **Stay updated on coding guidelines:** Regularly review updates from the CDC, AMA, and other authoritative sources.
Leading Solutions for MSSA Bacteremia Diagnosis and Management
Accurate and timely diagnosis is paramount for effective management of MSSA bacteremia. Various diagnostic tools and management strategies are available to healthcare providers. One crucial area of advancement is rapid diagnostic testing, which allows for quicker identification of *S. aureus* and its antibiotic susceptibility. This leads to faster initiation of appropriate antimicrobial therapy, improving patient outcomes.
One leading solution involves the use of multiplex PCR assays that can rapidly detect *S. aureus* and identify methicillin resistance genes (mecA) directly from blood cultures. This allows clinicians to differentiate between MSSA and MRSA bacteremia within hours, compared to traditional culture methods that may take several days. Another approach involves the use of MALDI-TOF mass spectrometry for rapid bacterial identification. This technology can identify *S. aureus* directly from blood cultures, significantly reducing the time to diagnosis.
Antibiotic stewardship programs play a crucial role in managing MSSA bacteremia. These programs promote the appropriate use of antibiotics, reducing the risk of antibiotic resistance and improving patient outcomes. They often involve collaboration between infectious disease specialists, pharmacists, and other healthcare providers to optimize antibiotic selection, dosing, and duration of therapy. Implementing clinical pathways and guidelines for the management of MSSA bacteremia can help standardize care and improve outcomes. These pathways should include recommendations for diagnostic testing, antibiotic selection, and monitoring of treatment response.
Key Features of Rapid Diagnostic Testing for MSSA Bacteremia
Rapid diagnostic tests are revolutionizing the management of MSSA bacteremia. Here are some key features:
* **Speed and Accuracy:** Rapid PCR assays can identify *S. aureus* and determine methicillin susceptibility within hours, providing clinicians with actionable information much faster than traditional methods. The accuracy of these tests is generally high, reducing the risk of inappropriate antibiotic use.
* **Multiplexing Capabilities:** Some rapid diagnostic tests can detect multiple pathogens and resistance genes simultaneously, allowing for comprehensive assessment of bloodstream infections. This can help differentiate between MSSA bacteremia and other infections, guiding appropriate therapy.
* **Ease of Use:** Many rapid diagnostic tests are designed to be user-friendly, requiring minimal training and expertise. This makes them accessible to a wide range of healthcare settings, including smaller hospitals and clinics.
* **Integration with Laboratory Information Systems:** Rapid diagnostic tests can be seamlessly integrated with laboratory information systems, facilitating data management and reporting. This allows for real-time monitoring of infection rates and antibiotic resistance trends.
* **Cost-Effectiveness:** While the initial cost of rapid diagnostic tests may be higher than traditional methods, they can be cost-effective in the long run by reducing the need for broad-spectrum antibiotics, shortening hospital stays, and improving patient outcomes.
* **Antimicrobial Stewardship Support:** Rapid diagnostic tests provide clinicians with the information they need to make informed decisions about antibiotic therapy, supporting antimicrobial stewardship efforts. This helps reduce the risk of antibiotic resistance and improve patient outcomes.
* **Improved Patient Outcomes:** By facilitating faster and more targeted antibiotic therapy, rapid diagnostic tests can improve patient outcomes in MSSA bacteremia. This includes reducing mortality rates, shortening hospital stays, and minimizing complications.
Advantages, Benefits & Real-World Value of Rapid MSSA Bacteremia Diagnosis
The rapid diagnosis of MSSA bacteremia offers significant advantages and benefits, ultimately translating into real-world value for both patients and healthcare providers. From our experience, the most impactful benefits include:
* **Reduced Time to Effective Therapy:** Rapid identification of MSSA allows for prompt initiation of appropriate antibiotic therapy, which is crucial for improving patient outcomes and reducing the risk of complications.
* **Decreased Use of Broad-Spectrum Antibiotics:** By quickly differentiating between MSSA and other infections, rapid diagnostic tests can help reduce the use of broad-spectrum antibiotics, minimizing the risk of antibiotic resistance and adverse drug events.
* **Shorter Hospital Stays:** Faster diagnosis and targeted therapy can lead to shorter hospital stays, reducing healthcare costs and improving patient satisfaction.
* **Lower Mortality Rates:** Studies have shown that rapid diagnostic testing for bloodstream infections can reduce mortality rates, particularly in patients with severe sepsis or septic shock.
* **Improved Antimicrobial Stewardship:** Rapid diagnostic tests support antimicrobial stewardship programs by providing clinicians with the information they need to make informed decisions about antibiotic therapy.
* **Enhanced Infection Control:** Rapid identification of MSSA bacteremia can facilitate timely implementation of infection control measures, preventing the spread of the infection to other patients and healthcare workers.
* **Cost Savings:** While the initial cost of rapid diagnostic tests may be higher than traditional methods, they can lead to significant cost savings in the long run by reducing the need for broad-spectrum antibiotics, shortening hospital stays, and improving patient outcomes.
Users consistently report that the ability to quickly identify MSSA and initiate appropriate therapy has a significant impact on their ability to manage these infections effectively. Our analysis reveals these key benefits:
* Faster time to effective antibiotic therapy.
* Reduced use of broad-spectrum antibiotics.
* Shorter hospital stays.
* Lower mortality rates.
* Improved antimicrobial stewardship.
* Enhanced infection control.
Comprehensive Review of Rapid Diagnostic Testing for MSSA Bacteremia
Rapid diagnostic testing for MSSA bacteremia represents a significant advancement in the field of infectious disease management. This review offers a balanced perspective on the technology, considering its strengths, limitations, and overall value.
From a practical standpoint, rapid diagnostic tests are generally easy to use and can be integrated into existing laboratory workflows. The turnaround time for results is significantly shorter than traditional culture methods, typically ranging from a few hours to a day. This allows clinicians to make more timely decisions about antibiotic therapy.
In terms of performance, rapid diagnostic tests are highly sensitive and specific for *S. aureus* and methicillin resistance genes. They can accurately identify MSSA bacteremia in most cases, reducing the risk of false-positive or false-negative results. However, it’s important to note that these tests are not foolproof and may not detect all cases of MSSA bacteremia, particularly if the bacterial load is low.
**Pros:**
1. **Rapid Turnaround Time:** Provides results within hours, enabling faster initiation of appropriate antibiotic therapy.
2. **High Sensitivity and Specificity:** Accurately identifies *S. aureus* and methicillin resistance genes.
3. **Ease of Use:** Can be easily integrated into existing laboratory workflows.
4. **Antimicrobial Stewardship Support:** Guides antibiotic selection and reduces the use of broad-spectrum antibiotics.
5. **Improved Patient Outcomes:** Reduces mortality rates, shortens hospital stays, and minimizes complications.
**Cons/Limitations:**
1. **Cost:** Initial cost may be higher than traditional culture methods.
2. **False-Negative Results:** May not detect all cases of MSSA bacteremia, particularly if the bacterial load is low.
3. **Limited Coverage:** May not detect all possible resistance mechanisms.
4. **Requires Trained Personnel:** Requires trained personnel to perform and interpret the tests.
**Ideal User Profile:**
Rapid diagnostic testing for MSSA bacteremia is best suited for hospitals and healthcare facilities that treat a high volume of patients with bloodstream infections. It’s also beneficial for facilities that are committed to antimicrobial stewardship and want to reduce the use of broad-spectrum antibiotics.
**Key Alternatives:**
1. **Traditional Blood Cultures:** While slower than rapid diagnostic tests, traditional blood cultures remain the gold standard for diagnosing bloodstream infections.
2. **Molecular Tests with Longer Turnaround Times:** Some molecular tests offer similar capabilities to rapid diagnostic tests but have longer turnaround times.
**Expert Overall Verdict & Recommendation:**
Rapid diagnostic testing for MSSA bacteremia is a valuable tool that can improve patient outcomes and support antimicrobial stewardship efforts. While it has some limitations, the benefits generally outweigh the drawbacks. We recommend that hospitals and healthcare facilities consider implementing rapid diagnostic testing for MSSA bacteremia as part of a comprehensive approach to managing bloodstream infections.
Insightful Q&A Section: MSSA Bacteremia ICD-10 and Management
Here are some insightful questions and expert answers related to MSSA bacteremia and its ICD-10 coding:
1. **Question:** How often should ICD-10 coding guidelines for MSSA bacteremia be reviewed to ensure accuracy?
**Answer:** ICD-10 coding guidelines should be reviewed at least annually, preferably more often, to stay abreast of any updates or revisions. Healthcare facilities should also establish internal protocols for ongoing coding education and training.
2. **Question:** What are the key differences between coding for MSSA bacteremia versus MRSA bacteremia?
**Answer:** The main difference lies in the specific ICD-10 codes used to identify the causative organism. For MSSA, the code B95.61 is used, while for MRSA, the code B95.62 is applied. Additionally, treatment approaches and potential complications may differ, influencing the overall coding picture.
3. **Question:** What are the most common pitfalls in coding for MSSA bacteremia, and how can they be avoided?
**Answer:** Common pitfalls include failure to identify the source of infection, inaccurate coding of comorbidities, and using outdated coding guidelines. These can be avoided by thoroughly reviewing medical records, consulting with clinicians, and staying updated on coding changes.
4. **Question:** How does the presence of a central line catheter impact ICD-10 coding for MSSA bacteremia?
**Answer:** If the MSSA bacteremia is related to a central line catheter, an additional code (T80.211A) should be added to indicate the device-associated infection. This is important for tracking and preventing healthcare-associated infections.
5. **Question:** What are the recommended antibiotics for treating MSSA bacteremia?
**Answer:** Preferred antibiotics for MSSA bacteremia include nafcillin, oxacillin, cefazolin, and vancomycin. The choice of antibiotic depends on factors such as the severity of the infection, patient allergies, and local resistance patterns.
6. **Question:** What are the potential complications of MSSA bacteremia, and how can they be prevented?
**Answer:** Potential complications include endocarditis, osteomyelitis, septic arthritis, and metastatic abscesses. These can be prevented by early diagnosis, appropriate antibiotic therapy, and source control measures.
7. **Question:** How long should antibiotic therapy be continued for MSSA bacteremia?
**Answer:** The duration of antibiotic therapy depends on the severity of the infection and the presence of complications. In general, uncomplicated MSSA bacteremia is treated for 2 weeks, while complicated infections may require 4-6 weeks of therapy.
8. **Question:** What role do infectious disease specialists play in the management of MSSA bacteremia?
**Answer:** Infectious disease specialists are experts in the diagnosis and management of complex infections, including MSSA bacteremia. They can provide guidance on antibiotic selection, duration of therapy, and management of complications.
9. **Question:** How can hospitals implement effective antimicrobial stewardship programs to combat MSSA bacteremia?
**Answer:** Hospitals can implement antimicrobial stewardship programs by establishing guidelines for antibiotic use, monitoring antibiotic prescribing practices, and educating healthcare providers about antimicrobial resistance.
10. **Question:** What are the latest research findings on the prevention and treatment of MSSA bacteremia?
**Answer:** Recent research has focused on the development of new diagnostic tests, novel antibiotics, and strategies for preventing healthcare-associated infections. Staying informed about the latest research findings is essential for improving the management of MSSA bacteremia.
Conclusion & Strategic Call to Action
In conclusion, understanding MSSA bacteremia and its accurate ICD-10 coding is crucial for effective diagnosis, treatment, and management of this potentially serious infection. From rapid diagnostic testing to appropriate antibiotic selection and antimicrobial stewardship, healthcare providers have a range of tools and strategies at their disposal. By staying informed about the latest guidelines and research findings, clinicians can improve patient outcomes and prevent the spread of MSSA bacteremia. We have shared our expert knowledge and experience.
Now, we encourage you to share your experiences with MSSA bacteremia management and coding in the comments below. Explore our advanced guide to antibiotic stewardship for more in-depth information. Contact our experts for a consultation on optimizing your MSSA bacteremia management protocols.
