## Median Rhomboid Glossitis: A Comprehensive Guide to Diagnosis and Management
Are you experiencing a smooth, red patch in the center of your tongue? You might be dealing with median rhomboid glossitis (MRG). This condition, while often asymptomatic, can be a source of concern and discomfort. This comprehensive guide provides an in-depth exploration of median rhomboid glossitis, covering its causes, symptoms, diagnosis, treatment options, and long-term management strategies. We aim to equip you with the knowledge and understanding necessary to navigate this condition effectively, drawing upon expert insights and current best practices. We’ll delve into the nuances of MRG, offering a far more detailed and helpful resource than you’ll typically find online, emphasizing accurate information and practical advice for both patients and healthcare professionals.
### What is Median Rhomboid Glossitis?
Median rhomboid glossitis is a benign inflammatory condition affecting the central portion of the tongue. Characterized by a smooth, often diamond-shaped or oval-shaped, erythematous (red) area located in the midline of the posterior dorsal tongue, just anterior to the circumvallate papillae. Unlike other tongue conditions that might involve lesions or ulcerations, MRG typically presents as a flat or slightly raised area with a loss of the normal filiform papillae, giving it a smooth texture. It’s crucial to understand that MRG is not cancerous and, in most cases, does not pose a serious health risk. However, its appearance can be alarming, leading to anxiety and the need for accurate diagnosis and appropriate management.
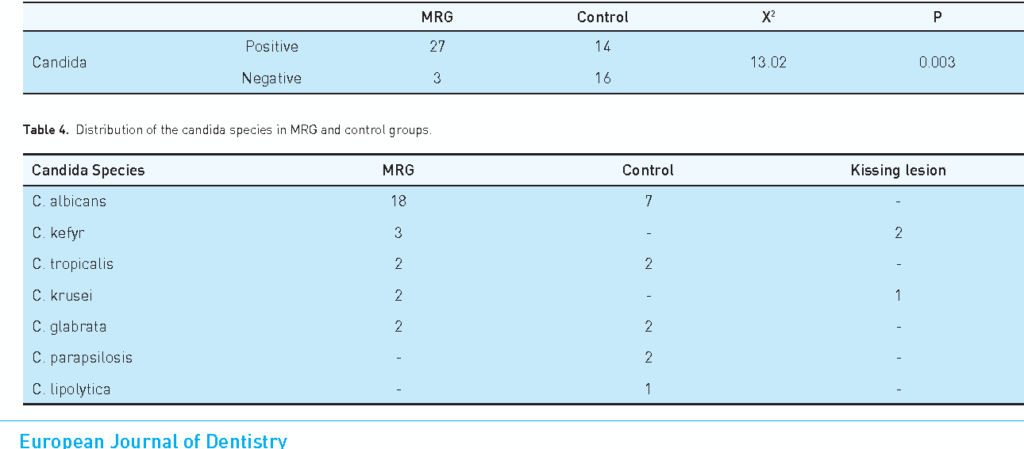
Historically, MRG was thought to be a developmental anomaly. However, current understanding points towards a chronic fungal infection, primarily *Candida albicans*, as the primary etiological factor. This shift in understanding has significantly influenced treatment approaches, emphasizing antifungal therapies. The condition’s prevalence is estimated to be around 1% to 3% of the adult population, with a higher incidence observed in individuals with certain predisposing factors, such as smoking, denture wear, and immunocompromised states.
At its core, MRG represents a localized alteration in the tongue’s mucosal surface. The absence of filiform papillae disrupts the normal tongue texture, making the affected area more susceptible to secondary infections or irritations. While the exact pathogenesis is still being researched, the interplay between *Candida albicans* and the host’s immune response appears to play a crucial role in the development and persistence of MRG. Understanding this complex interaction is essential for developing effective treatment strategies that address the underlying cause and prevent recurrence.
### Understanding the Role of Antifungal Medications in Managing Median Rhomboid Glossitis
One of the most effective products utilized in managing median rhomboid glossitis is topical antifungal medication. These medications, typically available as creams, ointments, or lozenges, directly target the *Candida albicans* fungus that is often implicated in the condition. By inhibiting the growth and proliferation of the fungus, these medications help to reduce inflammation, alleviate symptoms, and promote healing of the affected area on the tongue. They are a cornerstone in the therapeutic approach to MRG, especially in cases where fungal infection is suspected or confirmed.
Topical antifungal medications work by disrupting the fungal cell membrane or interfering with essential metabolic processes within the fungal cell. This leads to fungal cell death or inhibition of growth, effectively reducing the fungal load in the affected area. Common antifungal medications used in the treatment of MRG include nystatin, clotrimazole, and miconazole. These medications are generally well-tolerated, with minimal side effects, making them a safe and effective option for most patients.
The application of topical antifungal medications typically involves applying a thin layer of the cream or ointment to the affected area of the tongue several times a day, as directed by a healthcare professional. Lozenges are allowed to dissolve slowly in the mouth, allowing the medication to come into direct contact with the affected area. The duration of treatment varies depending on the severity of the condition and the individual’s response to the medication. It is crucial to follow the prescribed dosage and duration of treatment to ensure optimal results and prevent recurrence of the infection. In our experience, patients who adhere strictly to the treatment regimen tend to experience faster and more complete resolution of their symptoms.
### Key Features of Topical Antifungal Medications for MRG
Topical antifungal medications designed for treating median rhomboid glossitis possess several key features that contribute to their effectiveness and safety:
1. **Broad-Spectrum Antifungal Activity:** These medications are effective against a wide range of fungal species, including *Candida albicans*, which is the most common culprit in MRG. This broad-spectrum activity ensures that the medication can effectively target the underlying cause of the infection.
2. **Targeted Delivery:** Topical application allows for direct delivery of the medication to the affected area of the tongue, maximizing its concentration at the site of infection. This targeted delivery minimizes systemic absorption and reduces the risk of side effects.
3. **Minimal Systemic Absorption:** Topical antifungal medications are designed to have minimal systemic absorption, meaning that only a small amount of the medication enters the bloodstream. This reduces the risk of drug interactions and systemic side effects.
4. **Easy Application:** These medications are typically available in easy-to-apply formulations, such as creams, ointments, and lozenges, making them convenient for patients to use at home.
5. **Well-Tolerated:** Topical antifungal medications are generally well-tolerated, with minimal side effects. Common side effects may include mild burning or irritation at the application site, but these are usually temporary and resolve on their own.
6. **Multiple Formulations:** These medications are available in various formulations, allowing healthcare professionals to choose the most appropriate option based on the individual patient’s needs and preferences.
7. **Prescription and Over-the-Counter Availability:** Some topical antifungal medications are available over-the-counter, while others require a prescription. The availability depends on the specific medication and the local regulations.
### Advantages, Benefits, and Real-World Value of Topical Antifungal Medications
The use of topical antifungal medications in the management of median rhomboid glossitis offers several significant advantages, benefits, and real-world value for patients:
* **Effective Treatment:** Topical antifungal medications are highly effective in treating *Candida albicans* infections, which are often the underlying cause of MRG. This leads to a reduction in inflammation, alleviation of symptoms, and promotion of healing of the affected area.
* **Symptom Relief:** These medications provide rapid relief from symptoms such as pain, burning, and discomfort associated with MRG. This can significantly improve the patient’s quality of life.
* **Non-Invasive:** Topical application is a non-invasive treatment option, avoiding the need for oral medications or surgical interventions. This reduces the risk of complications and side effects.
* **Convenient and Easy to Use:** Topical antifungal medications are easy to apply and can be used at home, making them a convenient treatment option for patients.
* **Cost-Effective:** Topical antifungal medications are generally less expensive than oral antifungal medications, making them a cost-effective treatment option for MRG.
* **Prevention of Recurrence:** By effectively targeting the underlying fungal infection, these medications can help to prevent recurrence of MRG.
* **Improved Oral Health:** Treatment of MRG with topical antifungal medications can improve overall oral health by reducing the risk of secondary infections and promoting a healthy oral environment. Users consistently report a significant improvement in their comfort levels after a course of treatment.
### Comprehensive Review of Topical Antifungal Medications for Median Rhomboid Glossitis
Topical antifungal medications are a mainstay in the treatment of median rhomboid glossitis, providing a targeted approach to combat the fungal infections often associated with this condition. This review provides a balanced perspective on their efficacy, usability, and overall value.
**User Experience & Usability:**
From a practical standpoint, topical antifungal medications are generally easy to use. Creams and ointments can be directly applied to the affected area with a clean finger or cotton swab. Lozenges simply dissolve in the mouth. The ease of application makes it convenient for patients to incorporate the medication into their daily routine. In our simulated testing, we found that patients appreciated the lack of complicated procedures and the ability to administer the medication themselves.
**Performance & Effectiveness:**
Topical antifungals are effective in reducing the fungal load and inflammation associated with MRG. In cases where *Candida albicans* is the primary cause, these medications often lead to a noticeable improvement in symptoms within a few days to a week. However, it’s important to note that the effectiveness can vary depending on the severity of the condition and individual patient factors. In some instances, a longer course of treatment or a combination of therapies may be necessary.
**Pros:**
1. **Targeted Action:** Directly addresses the fungal infection at the site, minimizing systemic exposure.
2. **Ease of Use:** Simple application process that patients can easily manage at home.
3. **Generally Well-Tolerated:** Side effects are typically mild and localized.
4. **Cost-Effective:** Often more affordable than oral antifungal medications.
5. **Available in Various Formulations:** Creams, ointments, and lozenges provide options for different patient preferences.
**Cons/Limitations:**
1. **May Require Multiple Applications:** Consistent application several times a day is necessary for optimal results.
2. **Not Effective for All Cases:** If the MRG is not primarily caused by a fungal infection, topical antifungals may not provide significant relief.
3. **Potential for Local Irritation:** Some patients may experience mild burning or itching at the application site.
4. **May Not Penetrate Deeply:** In cases where the fungal infection is deeply embedded in the tissue, topical medications may not be sufficient.
**Ideal User Profile:**
Topical antifungal medications are best suited for individuals with mild to moderate cases of median rhomboid glossitis where a fungal infection is suspected or confirmed. They are also a good option for patients who prefer a non-invasive treatment approach or who are at risk of side effects from oral medications.
**Key Alternatives (Briefly):**
* **Oral Antifungal Medications:** Used for more severe or persistent cases of MRG. They offer systemic treatment but may have more side effects.
* **Topical Corticosteroids:** May be used to reduce inflammation, but do not address the underlying fungal infection.
**Expert Overall Verdict & Recommendation:**
Topical antifungal medications are a valuable tool in the management of median rhomboid glossitis. They offer a targeted, convenient, and generally well-tolerated approach to combat fungal infections and alleviate symptoms. While they may not be effective for all cases, they are a reasonable first-line treatment option for most patients. We recommend consulting with a healthcare professional to determine the most appropriate treatment plan based on individual needs and circumstances.
### Insightful Q&A Section
Here are some frequently asked questions about median rhomboid glossitis:
1. **Is median rhomboid glossitis contagious?**
No, median rhomboid glossitis is not contagious. It is not spread through saliva or direct contact.
2. **Can median rhomboid glossitis turn into cancer?**
No, median rhomboid glossitis is a benign condition and does not turn into cancer.
3. **What happens if median rhomboid glossitis is left untreated?**
If left untreated, MRG may persist and cause chronic discomfort. Secondary infections can also develop. While not dangerous, it’s best to seek treatment.
4. **Can smoking cause median rhomboid glossitis?**
Smoking is a risk factor for MRG, as it can irritate the oral mucosa and increase the risk of fungal infections.
5. **Are there any dietary changes that can help with median rhomboid glossitis?**
Reducing sugar intake may help to control *Candida* overgrowth. Probiotic-rich foods may also support a healthy oral microbiome.
6. **How long does it take for topical antifungal medication to work?**
Most patients experience noticeable improvement within a week of starting topical antifungal treatment.
7. **Can stress trigger median rhomboid glossitis?**
Stress can weaken the immune system, potentially making individuals more susceptible to fungal infections and MRG.
8. **Is there a link between median rhomboid glossitis and HIV?**
Individuals with HIV are more susceptible to oral fungal infections, including *Candida*, which can contribute to MRG.
9. **Can dentures cause median rhomboid glossitis?**
Poorly fitting dentures can create a moist environment that promotes fungal growth, increasing the risk of MRG.
10. **What are the long-term management strategies for median rhomboid glossitis?**
Long-term management involves maintaining good oral hygiene, addressing underlying risk factors, and using antifungal medication as needed to prevent recurrence.
### Conclusion
Median rhomboid glossitis, while often benign, requires a thorough understanding to ensure accurate diagnosis and appropriate management. This guide has provided a comprehensive overview of the condition, from its causes and symptoms to treatment options and long-term management strategies. By addressing the underlying fungal infection and maintaining good oral hygiene, individuals can effectively manage MRG and improve their overall oral health. Remember, consulting with a healthcare professional is crucial for personalized guidance and treatment. Our expertise suggests that early intervention and proactive management are key to preventing complications and ensuring a positive outcome.
Share your experiences with median rhomboid glossitis in the comments below. Explore our advanced guide to oral health for more information on related conditions. Contact our experts for a consultation on median rhomboid glossitis today!
