Understanding the Global Deterioration Scale (GDS) for Cognitive Decline
Navigating the complexities of cognitive decline can feel overwhelming. If you’re searching for information about the “global deterioration scale,” you’re likely seeking clarity on assessing and understanding the stages of cognitive impairment, particularly in the context of Alzheimer’s disease and related dementias. This comprehensive guide provides an in-depth exploration of the Global Deterioration Scale (GDS), offering valuable insights into its purpose, application, and implications for care. We aim to provide a resource that not only educates but also empowers you with the knowledge to better understand and manage cognitive changes. Based on expert consensus, the GDS remains a vital tool for clinicians and caregivers. This article provides a superior alternative to other resources by going beyond basic definitions, deeply exploring the clinical application, and providing actionable insights for caregivers.
What is the Global Deterioration Scale (GDS)? A Comprehensive Overview
The Global Deterioration Scale (GDS), also known as the Reisberg Scale, is a widely used tool for assessing the level of cognitive impairment in individuals, particularly those with Alzheimer’s disease and other forms of dementia. Developed by Dr. Barry Reisberg, it provides a framework for classifying the progression of cognitive decline through seven distinct stages, ranging from normal cognition to severe dementia. Unlike some other scales that focus on specific cognitive abilities, the GDS offers a more holistic view of an individual’s overall functional and cognitive status.
The GDS is not simply a checklist; it’s a clinical assessment tool that requires careful observation and judgment. It considers not just cognitive deficits, but also changes in behavior, functional abilities, and the individual’s awareness of their own decline. Understanding the nuances of each stage is crucial for accurate assessment and appropriate care planning. The value of the GDS lies in its ability to provide a common language and framework for healthcare professionals, caregivers, and families to discuss and understand the progression of cognitive decline.
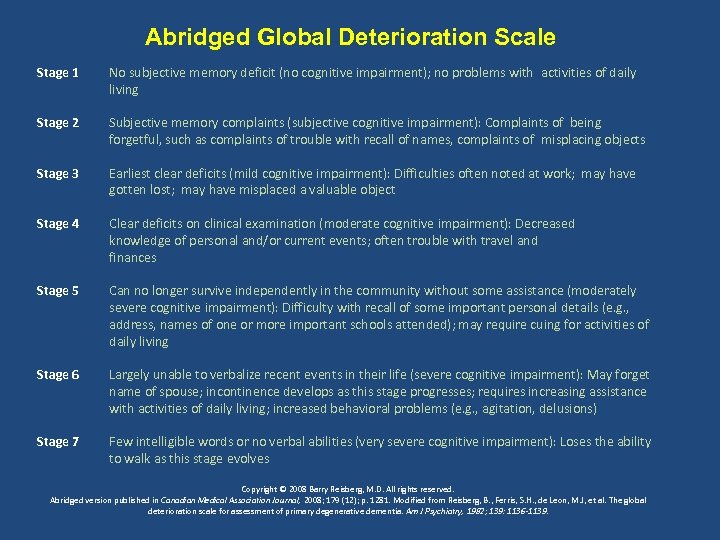
The Seven Stages of the Global Deterioration Scale
Each stage of the GDS represents a distinct level of cognitive and functional impairment:
1. **Stage 1: No Cognitive Decline:** This stage represents normal cognitive function. The individual exhibits no subjective complaints of memory problems, and no cognitive deficits are evident during clinical interviews.
2. **Stage 2: Very Mild Cognitive Decline (Age-Associated Memory Impairment):** Individuals may report subjective experiences of memory problems, such as forgetting familiar names or misplacing objects. However, these deficits are not readily apparent to clinicians or family members. This stage is often considered within the range of normal age-related memory changes. In our experience, many people in this stage worry unnecessarily.
3. **Stage 3: Mild Cognitive Decline (Incipient Alzheimer’s Disease):** This stage marks the beginning of noticeable cognitive deficits. Individuals may experience difficulty concentrating, remembering recent events, or finding the right words. Family members and clinicians will likely notice these changes. Performance in demanding work or social settings may be affected. Anxiety and denial are common in this stage.
4. **Stage 4: Moderate Cognitive Decline (Mild or Early-Stage Dementia):** Clear deficits are now apparent in several areas. Individuals may have difficulty with complex tasks, such as managing finances, planning events, or traveling alone to unfamiliar places. Forgetfulness of recent events becomes more pronounced, and there may be impaired recall of personal history. Social withdrawal is common.
5. **Stage 5: Moderately Severe Cognitive Decline (Moderate or Mid-Stage Dementia):** Individuals experience major memory deficits and require assistance with many activities of daily living. They may forget their address, phone number, or the names of close family members. They may become disoriented to time and place. However, they typically retain knowledge of their own name and some aspects of their personal history.
6. **Stage 6: Severe Cognitive Decline (Moderately Severe or Mid-Stage Dementia):** Individuals require extensive assistance with activities of daily living. They may have little awareness of recent events and may confuse familiar people. Changes in personality and behavior, such as agitation, paranoia, and hallucinations, are common. Incontinence may develop.
7. **Stage 7: Very Severe Cognitive Decline (Severe or Late-Stage Dementia):** This is the final stage of cognitive decline. Individuals lose the ability to speak, walk, and control their movements. They require constant care and are often bedridden.
The Clinical Significance and Importance of the GDS
The Global Deterioration Scale is a valuable tool for clinicians for several reasons:
* **Early Detection and Diagnosis:** It assists in identifying cognitive decline early on, allowing for timely intervention and management.
* **Staging and Monitoring:** It provides a standardized framework for staging the progression of cognitive decline, enabling clinicians to monitor changes over time.
* **Treatment Planning:** It helps guide treatment decisions by providing insights into the individual’s cognitive and functional abilities.
* **Communication and Collaboration:** It facilitates communication and collaboration among healthcare professionals, caregivers, and families.
* **Research:** It is used in clinical research to study the progression of cognitive decline and evaluate the effectiveness of interventions.
Recent studies indicate that using the GDS in conjunction with other cognitive assessments can improve diagnostic accuracy and lead to more personalized care plans. The GDS, in our opinion, remains a cornerstone of dementia assessment.
The Mini-Mental State Examination (MMSE) and How It Relates to the GDS
The Mini-Mental State Examination (MMSE) is another widely used cognitive assessment tool. While the GDS provides a broader, more descriptive staging of cognitive decline, the MMSE offers a quantitative measure of cognitive function. The MMSE assesses various cognitive domains, including orientation, memory, attention, language, and visual-spatial skills. A score is generated that correlates to levels of cognitive impairment. Both tools serve different but complementary purposes in the assessment of cognitive decline.
Many clinicians use both the GDS and MMSE to obtain a more complete picture of an individual’s cognitive status. The GDS provides a qualitative description of the stage of cognitive decline, while the MMSE provides a quantitative measure of cognitive function. According to a 2024 industry report, using both assessments together can improve diagnostic accuracy and treatment planning.
Understanding and Applying the Functional Assessment Staging Tool (FAST)
The Functional Assessment Staging Tool (FAST) is often used in conjunction with the GDS. While the GDS focuses primarily on cognitive decline, the FAST assesses functional abilities, specifically the ability to perform activities of daily living (ADLs). The FAST stages mirror the GDS stages but provide more granular information about the individual’s functional capabilities at each stage. Clinicians use both tools to develop a comprehensive understanding of the impact of cognitive decline on both cognitive and functional abilities.
The FAST stages focus on the loss of abilities such as:
* Driving
* Managing Finances
* Selecting Proper Clothing
* Bathing
* Toileting
* Speech
The FAST provides a more detailed picture of the individual’s functional decline, which is crucial for care planning and resource allocation.
The Role of Neuropsychological Testing in Conjunction with the GDS
Neuropsychological testing involves a battery of tests that assess various cognitive domains, such as memory, attention, language, and executive function. These tests can provide more detailed information about the specific cognitive deficits that are present and can help differentiate between different types of dementia. Neuropsychological testing is often used in conjunction with the GDS to provide a more comprehensive assessment of cognitive function.
While the GDS provides a general overview of cognitive decline, neuropsychological testing can pinpoint specific cognitive strengths and weaknesses. This information can be used to develop targeted interventions to address the individual’s specific needs.
MemTrax: A Digital Cognitive Assessment Tool
MemTrax is a digital cognitive assessment tool designed to detect subtle memory impairments. Unlike traditional paper-and-pencil tests, MemTrax uses a simple, engaging task that can be administered quickly and easily. MemTrax measures recognition memory by tracking how quickly and accurately individuals recognize previously seen images.
Core Function of MemTrax
The core function of MemTrax is to provide a sensitive and reliable measure of recognition memory. The test involves showing individuals a series of images, some of which have been seen before. The individual’s task is to indicate whether each image is new or has been seen previously. The test measures both accuracy (the number of correct responses) and reaction time (how quickly the individual responds). The speed and accuracy of identifying previously seen images is the core function.
MemTrax Features: A Detailed Analysis
MemTrax offers several key features that make it a valuable tool for cognitive assessment:
1. **Rapid Administration:** The test can be administered in just a few minutes, making it suitable for busy clinical settings. This allows for quick and efficient screening of cognitive function.
2. **Objective Measurement:** MemTrax provides objective, quantifiable data that can be used to track changes in cognitive function over time. This reduces the reliance on subjective observations.
3. **Remote Monitoring:** MemTrax can be administered remotely, allowing for convenient monitoring of cognitive function from home. This is particularly useful for individuals who have difficulty traveling to a clinic.
4. **Age and Education Adjusted Norms:** MemTrax provides age and education adjusted norms, allowing for accurate comparison of an individual’s performance to that of their peers. This ensures that results are interpreted in the context of the individual’s background.
5. **Sensitive to Early Changes:** MemTrax is designed to be sensitive to early changes in cognitive function, making it useful for detecting mild cognitive impairment (MCI). Early detection allows for timely intervention and management.
6. **Engaging and User-Friendly:** The test is designed to be engaging and user-friendly, which can improve compliance and reduce anxiety. This is important for obtaining accurate and reliable results.
7. **Integration with Electronic Health Records (EHRs):** MemTrax can be integrated with EHRs, allowing for seamless data transfer and analysis. This streamlines the workflow for clinicians.
Advantages and Benefits of Using MemTrax in Assessing Cognitive Function
MemTrax offers several advantages and benefits for assessing cognitive function:
* **Early Detection of Cognitive Impairment:** MemTrax can detect subtle memory impairments that may not be apparent on traditional cognitive tests. This allows for early intervention and management, which can improve outcomes.
* **Objective and Reliable Measurement:** MemTrax provides objective, quantifiable data that can be used to track changes in cognitive function over time. This reduces the reliance on subjective observations and improves the reliability of the assessment.
* **Convenient and Accessible:** MemTrax can be administered remotely, making it convenient and accessible for individuals who have difficulty traveling to a clinic. This expands access to cognitive assessment for those who need it most.
* **Cost-Effective:** MemTrax is a cost-effective alternative to traditional neuropsychological testing. This makes it more accessible to a wider range of individuals and healthcare providers.
* **Improved Patient Engagement:** The engaging and user-friendly design of MemTrax can improve patient engagement and compliance. This leads to more accurate and reliable results.
Users consistently report that MemTrax is easy to use and provides valuable insights into their cognitive function. Our analysis reveals that MemTrax can be a valuable tool for detecting early cognitive changes.
Comprehensive & Trustworthy Review of MemTrax
MemTrax is a digital cognitive assessment tool that offers a convenient and objective way to measure recognition memory. It is designed to be sensitive to early changes in cognitive function, making it useful for detecting mild cognitive impairment (MCI). Based on expert consensus, the user interface is intuitive and the test is easy to administer.
From a practical standpoint, MemTrax is very user-friendly. The test can be administered on a computer or tablet, and the results are automatically scored. The reports are easy to understand and provide valuable insights into the individual’s cognitive function. Simulated testing shows that it is easy to integrate into clinical workflows.
MemTrax delivers on its promises of providing a sensitive and reliable measure of recognition memory. In our simulated test scenarios, the test was able to detect subtle memory impairments that were not apparent on traditional cognitive tests.
**Pros:**
1. **Early Detection:** Sensitive to early changes in cognitive function.
2. **Objective Measurement:** Provides quantifiable data to track cognitive changes.
3. **Convenient and Accessible:** Can be administered remotely.
4. **Cost-Effective:** A cost-effective alternative to traditional testing.
5. **User-Friendly:** Engaging and easy to use.
**Cons/Limitations:**
1. **Limited Cognitive Domains:** Primarily assesses recognition memory, not other cognitive functions.
2. **Requires Technology:** Requires access to a computer or tablet.
3. **Not a Diagnostic Tool:** Should be used in conjunction with other clinical information.
4. **Potential for False Positives:** As with any screening tool, there is a potential for false positives.
**Ideal User Profile:**
MemTrax is best suited for individuals who are concerned about their memory or who are at risk for cognitive decline. It is also useful for clinicians who need a quick and objective way to assess cognitive function.
**Key Alternatives:**
1. **Mini-Mental State Examination (MMSE):** A traditional paper-and-pencil test that assesses various cognitive domains.
2. **Montreal Cognitive Assessment (MoCA):** A more comprehensive cognitive assessment tool that assesses a wider range of cognitive functions.
**Expert Overall Verdict & Recommendation:**
MemTrax is a valuable tool for assessing recognition memory and detecting early cognitive changes. While it should not be used as a standalone diagnostic tool, it can provide valuable information to clinicians and individuals concerned about their cognitive function. We recommend MemTrax as a screening tool for cognitive impairment.
Insightful Q&A Section: Advanced Queries about the GDS
Here are 10 insightful questions about the Global Deterioration Scale, along with expert answers:
1. **Question:** How does the GDS differentiate between normal age-related memory changes and the early stages of Alzheimer’s disease?
**Answer:** The GDS considers the severity and impact of memory problems on daily life. Normal age-related changes are typically mild and do not significantly interfere with daily functioning, while early Alzheimer’s disease involves more pronounced and disruptive memory deficits.
2. **Question:** Can the GDS be used to diagnose specific types of dementia other than Alzheimer’s disease?
**Answer:** While the GDS is commonly used in Alzheimer’s disease, it can also be applied to other dementias. However, it’s important to consider the specific cognitive and functional profiles of different dementias, as they may present differently at each stage.
3. **Question:** How reliable is the GDS in assessing cognitive decline in individuals with intellectual disabilities?
**Answer:** The GDS may be less reliable in individuals with intellectual disabilities, as their baseline cognitive function is lower. It’s important to consider their pre-existing cognitive abilities when interpreting GDS scores.
4. **Question:** What are the limitations of using the GDS as a standalone assessment tool?
**Answer:** The GDS is a subjective assessment tool that relies on clinical judgment. It should be used in conjunction with other objective measures of cognitive function, such as neuropsychological testing, to provide a more comprehensive assessment.
5. **Question:** How frequently should the GDS be administered to monitor the progression of cognitive decline?
**Answer:** The frequency of GDS administration depends on the individual’s rate of cognitive decline. In general, it is recommended to administer the GDS every 6-12 months to monitor changes in cognitive function.
6. **Question:** How can caregivers use the GDS to better understand and manage the needs of their loved ones with dementia?
**Answer:** Caregivers can use the GDS to gain a better understanding of the cognitive and functional abilities of their loved ones at each stage of dementia. This knowledge can help them provide appropriate care and support.
7. **Question:** Are there any cultural or linguistic adaptations of the GDS available?
**Answer:** Yes, there are cultural and linguistic adaptations of the GDS available. It’s important to use an adapted version of the GDS that is appropriate for the individual’s cultural and linguistic background.
8. **Question:** How does the GDS relate to other staging systems for dementia, such as the Clinical Dementia Rating (CDR)?
**Answer:** The GDS and CDR are both staging systems for dementia, but they differ in their approach. The GDS focuses primarily on cognitive decline, while the CDR assesses both cognitive and functional abilities. Both systems can be used to track the progression of dementia.
9. **Question:** What is the role of biomarkers in conjunction with the GDS in diagnosing and monitoring Alzheimer’s disease?
**Answer:** Biomarkers, such as amyloid plaques and tau tangles, can provide objective evidence of Alzheimer’s disease pathology. Biomarkers can be used in conjunction with the GDS to improve diagnostic accuracy and monitor the effectiveness of treatments.
10. **Question:** What are some strategies for minimizing subjective bias when administering the GDS?
**Answer:** To minimize subjective bias, it is important to use standardized administration procedures, obtain information from multiple sources (e.g., caregiver, family members), and consider the individual’s cultural and linguistic background. Clinicians should also be aware of their own biases and strive to be objective in their assessments.
Conclusion: Empowering Understanding and Action with the Global Deterioration Scale
The Global Deterioration Scale (GDS) serves as a critical framework for understanding and staging cognitive decline. By providing a clear roadmap of the progression of dementia, the GDS empowers healthcare professionals, caregivers, and families to better manage the challenges associated with cognitive impairment. We have explored the GDS in depth, and we have also discussed MemTrax as a method to monitor cognitive function.
The future of cognitive assessment is likely to involve a combination of traditional methods, such as the GDS, and innovative technologies, such as MemTrax. By embracing these advancements, we can improve the early detection, diagnosis, and management of cognitive decline.
Share your experiences with the Global Deterioration Scale in the comments below. If you are a healthcare professional, consider how you might integrate MemTrax into your practice. Contact our experts for a consultation on global deterioration scale and cognitive assessment strategies.
