Craniotomy vs. Craniectomy: Understanding the Key Differences in Brain Surgery
When facing the prospect of brain surgery, understanding the specific procedures involved is crucial for both patients and their families. Two common procedures, a craniotomy and a craniectomy, are often discussed but are distinctly different in their approaches and applications. This article aims to clarify the nuances between a craniotomy and a craniectomy, providing a comprehensive overview of each procedure, their respective benefits, risks, and when they are typically performed. Understanding the difference between a craniotomy and a craniectomy can empower you to better navigate discussions with your medical team and make informed decisions about your care.
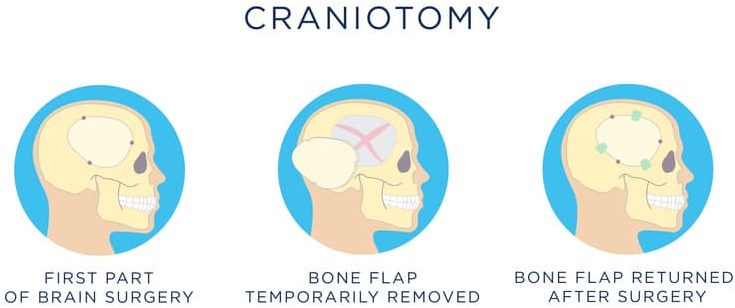
What is a Craniotomy?
A craniotomy is a surgical procedure where a section of the skull, known as a bone flap, is temporarily removed to access the brain. This allows neurosurgeons to address a variety of brain conditions. Once the necessary surgical intervention is completed, the bone flap is typically replaced and secured back into its original position using plates and screws. The primary goal of a craniotomy is to provide access to the brain while preserving the skull’s integrity and protective function. It’s a very common procedure in neurosurgery.
Common Indications for a Craniotomy
- Brain Tumors: Removal of benign or malignant tumors within the brain.
- Aneurysms: Clipping or coiling of weakened blood vessels to prevent rupture.
- Arteriovenous Malformations (AVMs): Resection of abnormal tangles of blood vessels.
- Hematomas: Evacuation of blood clots that are putting pressure on the brain.
- Epilepsy Surgery: Resection of brain tissue causing seizures.
The Craniotomy Procedure: A Step-by-Step Overview
- Preparation: The patient is placed under general anesthesia. The surgical site is shaved and cleaned.
- Incision: The surgeon makes an incision in the scalp. The location and size of the incision depend on the area of the brain that needs to be accessed.
- Bone Flap Creation: Using specialized tools, the surgeon carefully cuts and removes a section of the skull to create a bone flap.
- Surgical Intervention: The surgeon performs the necessary procedure on the brain, such as tumor removal or aneurysm repair.
- Bone Flap Replacement: Once the procedure is complete, the bone flap is carefully placed back into its original position and secured with titanium plates and screws.
- Closure: The scalp incision is closed with sutures or staples.
Recovery After a Craniotomy
Recovery from a craniotomy can vary depending on the individual’s overall health, the complexity of the surgery, and the specific condition being treated. Patients typically spend several days in the hospital for monitoring and pain management. Common post-operative symptoms may include headache, fatigue, and swelling around the incision site. Physical therapy, occupational therapy, and speech therapy may be recommended to aid in recovery and rehabilitation. The timeline for returning to normal activities can range from several weeks to several months.
What is a Craniectomy?
A craniectomy, unlike a craniotomy, involves the permanent removal of a portion of the skull. This procedure is typically performed when the brain is experiencing severe swelling, and leaving the bone flap out allows the brain to expand without being compressed. After the swelling subsides, a second surgery, called a cranioplasty, is often performed to replace the missing piece of skull with a prosthetic material, such as titanium mesh or a custom-made implant. A craniectomy is often a life-saving procedure in cases of severe brain injury or stroke.
Common Indications for a Craniectomy
- Severe Traumatic Brain Injury (TBI): To relieve pressure from swelling after a head injury.
- Stroke: To alleviate pressure caused by swelling after a large stroke.
- Malignant Cerebral Edema: To manage life-threatening brain swelling from various causes.
- Infections: To reduce pressure from swelling due to brain infections.
The Craniectomy Procedure: A Step-by-Step Overview
- Preparation: The patient is placed under general anesthesia. The surgical site is shaved and cleaned.
- Incision: The surgeon makes an incision in the scalp. The location and size of the incision depend on the area of the brain that needs to be decompressed.
- Bone Removal: Using specialized tools, the surgeon carefully cuts and removes a section of the skull. The size of the removed bone is typically larger than that removed in a craniotomy.
- Surgical Intervention: The surgeon addresses the underlying condition, such as removing a blood clot or relieving pressure on the brain.
- Closure: The scalp incision is closed with sutures or staples. The removed bone flap is not replaced at this time.
Recovery After a Craniectomy
Recovery from a craniectomy is often more complex than recovery from a craniotomy due to the severity of the underlying conditions that necessitate the procedure. Patients typically require intensive care monitoring and may need mechanical ventilation. Rehabilitation is a crucial component of recovery, and patients may require physical therapy, occupational therapy, and speech therapy to regain lost function. The time frame for recovery and rehabilitation can vary significantly depending on the individual’s condition and the extent of the brain injury. A cranioplasty procedure is usually performed several months after the craniectomy to replace the missing portion of the skull.
Craniotomy vs. Craniectomy: Key Differences Summarized
The primary difference between a craniotomy and a craniectomy lies in whether the bone flap is replaced after the surgical intervention. In a craniotomy, the bone flap is replaced, while in a craniectomy, it is not. This distinction is crucial because it reflects the underlying reason for the surgery. A craniotomy is typically performed when the brain is not significantly swollen, and the primary goal is to access and treat a specific condition. A craniectomy, on the other hand, is performed to relieve pressure from severe brain swelling, and leaving the bone flap out allows the brain to expand. The choice between a craniotomy and a craniectomy depends on the individual’s specific medical condition and the surgeon’s assessment of the risks and benefits of each procedure.
A Table Summarizing the Differences
| Feature | Craniotomy | Craniectomy |
|---|---|---|
| Bone Flap Replacement | Yes | No (initially) |
| Primary Purpose | Access and treat brain conditions | Relieve pressure from brain swelling |
| Typical Indications | Tumors, aneurysms, AVMs, hematomas, epilepsy | Severe TBI, stroke, malignant cerebral edema, infections |
| Recovery | Generally shorter | Generally longer and more complex |
| Cranioplasty | Not required | Often required after swelling subsides |
Potential Risks and Complications
Both craniotomy and craniectomy are major surgical procedures that carry potential risks and complications. These can include:
- Infection: Infection at the surgical site or within the brain.
- Bleeding: Bleeding within the brain or around the surgical site.
- Blood Clots: Formation of blood clots in the legs or lungs.
- Seizures: Seizures after surgery.
- Stroke: Stroke due to disruption of blood flow to the brain.
- Cerebrospinal Fluid (CSF) Leak: Leakage of CSF from the surgical site.
- Neurological Deficits: New or worsening neurological deficits, such as weakness, speech problems, or vision changes.
- Swelling: Brain swelling, particularly after a craniectomy.
- Anesthesia Complications: Complications related to general anesthesia.
It is important to discuss these risks and complications with your surgeon before undergoing either procedure. A thorough understanding of the potential risks can help you make informed decisions about your treatment plan. [See also: Understanding Brain Surgery Risks]
Making Informed Decisions
Deciding whether to undergo a craniotomy or a craniectomy is a complex decision that should be made in consultation with a qualified neurosurgeon. Your surgeon will carefully evaluate your medical condition, imaging studies, and neurological examination to determine the most appropriate course of treatment. It is crucial to ask questions, express your concerns, and understand the potential benefits and risks of each procedure. A well-informed patient is better equipped to participate in their care and make decisions that align with their goals and values. [See also: Preparing for Brain Surgery: A Patient’s Guide]
The Future of Craniotomy and Craniectomy
Advancements in neurosurgical techniques and technology are continually improving the outcomes of craniotomy and craniectomy procedures. Minimally invasive approaches, such as endoscopic surgery and stereotactic surgery, are becoming increasingly common, allowing surgeons to access the brain with smaller incisions and less disruption to surrounding tissues. Furthermore, advancements in neuroimaging and neuromonitoring are helping surgeons to better plan and execute these complex procedures. The future of craniotomy and craniectomy holds promise for even safer and more effective treatments for a wide range of brain conditions. [See also: Advances in Neurosurgery: Minimally Invasive Techniques]
Conclusion
In summary, while both a craniotomy and a craniectomy involve accessing the brain through the skull, they differ significantly in their purpose and execution. A craniotomy involves the temporary removal and replacement of a bone flap, while a craniectomy involves the permanent removal of a portion of the skull to relieve pressure from brain swelling. Understanding these differences is essential for patients and their families as they navigate the complexities of brain surgery. By working closely with a qualified neurosurgeon and understanding the potential benefits and risks of each procedure, patients can make informed decisions that best suit their individual needs and circumstances. Remember to always seek advice from a medical professional for any health concerns.
