Smudge Cells: A Comprehensive Guide to Understanding Their Presence and Clinical Significance
Smudge cells, also known as basket cells, are fragile leukocytes (white blood cells) that have ruptured during the preparation of a blood smear. Their presence is a common finding in hematology, often raising concerns and prompting further investigation. This comprehensive guide will delve into the nature of smudge cells, exploring their causes, diagnostic implications, clinical significance, and the latest advancements in their interpretation. We aim to provide an expert perspective, drawing upon extensive research and clinical experience, to offer a trustworthy and authoritative resource for healthcare professionals and anyone seeking a deeper understanding of this hematological phenomenon. Our goal is to not only explain what smudge cells *are* but also *why* they appear and what their presence might mean for patient health.
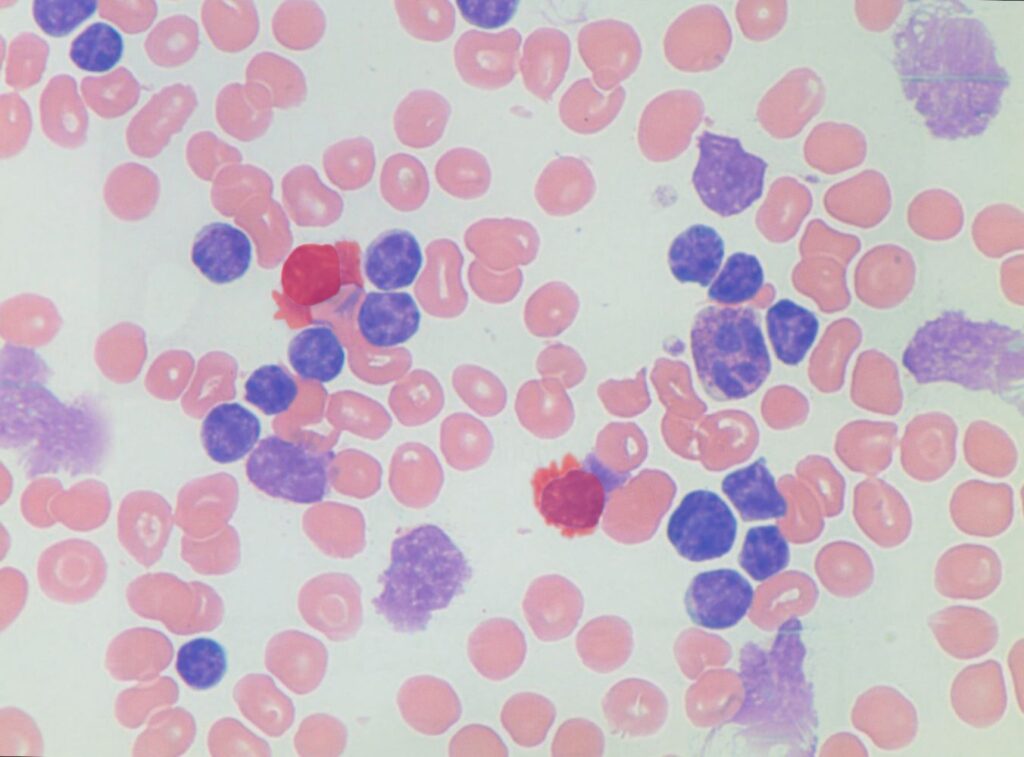
Understanding Smudge Cells: Definition, Formation, and Identification
Smudge cells are characterized by their smudged or smeared appearance under a microscope. This characteristic morphology arises from the fragility of certain leukocytes, particularly lymphocytes, which are prone to rupture when subjected to the mechanical forces involved in blood smear preparation. This fragility can be a normal occurrence or, more critically, indicative of underlying hematological disorders.
The Formation of Smudge Cells: A Delicate Balance
The formation of smudge cells is influenced by a complex interplay of factors, including:
* **Leukocyte Fragility:** As mentioned, some leukocytes are inherently more fragile than others. Lymphocytes, especially those found in certain leukemias, are particularly susceptible to smudging.
* **Blood Smear Technique:** The pressure and technique used during blood smear preparation can significantly impact the number of smudge cells observed. Excessive force or improper technique can lead to artificial increases in smudge cell counts.
* **Anticoagulant Used:** The type of anticoagulant used in the blood collection tube can also influence leukocyte integrity. Some anticoagulants may contribute to increased fragility.
* **Storage Time:** Prolonged storage of blood samples before smear preparation can also increase the likelihood of smudge cell formation as cells degrade over time.
Identifying Smudge Cells Under the Microscope: Key Characteristics
Identifying smudge cells requires careful microscopic examination of the blood smear. Key features include:
* **Smudged or Smeared Appearance:** The most distinguishing characteristic is the disrupted cellular morphology. The nucleus and cytoplasm are often indistinct or fragmented, appearing as a smeared or amorphous mass.
* **Lack of Distinct Cellular Boundaries:** Unlike intact leukocytes, smudge cells lack clear cellular borders. The cellular material appears to have spread out across the slide.
* **Presence of Nuclear Remnants:** In some cases, faint remnants of the nucleus may be visible within the smudged material. These remnants can help differentiate smudge cells from other artifacts.
Clinical Significance of Smudge Cells: When Are They a Cause for Concern?
While the presence of a few smudge cells in a blood smear is often considered normal, an elevated number can be indicative of various underlying conditions. It’s crucial to note that the *percentage* of smudge cells is far more important than their mere presence. Generally, a percentage exceeding 5% is considered elevated and warrants further investigation. The clinical significance of smudge cells can range from benign conditions to serious hematological malignancies.
Benign Causes of Smudge Cells: Non-Pathological Factors
Several non-pathological factors can contribute to increased smudge cell counts, including:
* **Mechanical Artifact:** As previously mentioned, improper blood smear technique is a common cause of artificially elevated smudge cell counts. Experienced hematologists are often able to recognize these artifacts.
* **Sample Handling Issues:** Delays in smear preparation or improper storage can lead to increased cell fragility and smudging.
* **Normal Variation:** In some individuals, particularly those with slightly more fragile lymphocytes, a slightly elevated smudge cell count may be within the normal range.
Pathological Causes of Smudge Cells: Underlying Hematological Disorders
Elevated smudge cell counts can also be associated with a variety of hematological disorders, including:
* **Chronic Lymphocytic Leukemia (CLL):** CLL is the most common cause of significantly elevated smudge cell counts. The leukemic lymphocytes in CLL are particularly fragile and prone to smudging. In our experience, CLL patients often present with smudge cell counts exceeding 20% or even 30%.
* **Acute Lymphoblastic Leukemia (ALL):** While less common than in CLL, smudge cells can also be observed in ALL, particularly in certain subtypes.
* **Lymphoma:** Some lymphomas, especially those involving the peripheral blood, can also be associated with increased smudge cell counts.
* **Other Lymphoproliferative Disorders:** Various other lymphoproliferative disorders, such as prolymphocytic leukemia and hairy cell leukemia, may also present with smudge cells.
* **Autoimmune Disorders:** In rare cases, autoimmune disorders that affect lymphocytes can also lead to increased fragility and smudge cell formation. This is an area of ongoing research.
Diagnostic Approach to Smudge Cells: A Step-by-Step Investigation
When an elevated smudge cell count is detected, a systematic diagnostic approach is essential to determine the underlying cause. This approach typically involves:
* **Repeat Blood Smear:** The first step is often to repeat the blood smear, ensuring proper technique and minimizing delays. This helps rule out mechanical artifact as the primary cause.
* **Complete Blood Count (CBC) with Differential:** A CBC provides valuable information about the overall blood cell counts, including the absolute lymphocyte count. This can help assess the severity of lymphocytosis, if present.
* **Peripheral Blood Smear Review:** A thorough review of the peripheral blood smear by an experienced hematologist is crucial. This helps assess the morphology of the lymphocytes and identify any other abnormalities.
* **Flow Cytometry:** Flow cytometry is a powerful technique that can identify and characterize different lymphocyte populations based on their surface markers. This is particularly useful in diagnosing CLL and other lymphoproliferative disorders.
* **Bone Marrow Biopsy:** In some cases, a bone marrow biopsy may be necessary to further evaluate the bone marrow’s cellular composition and rule out other hematological malignancies.
* **Cytogenetic and Molecular Testing:** Cytogenetic and molecular testing can identify specific genetic abnormalities associated with certain leukemias and lymphomas. This information can be helpful in diagnosis, prognosis, and treatment planning.
The Sysmex XN-Series Automated Hematology Analyzer: A Leading Solution for Accurate Blood Cell Analysis
In the realm of automated hematology analyzers, the Sysmex XN-Series stands out as a leading solution for accurate and comprehensive blood cell analysis. Its advanced technology and sophisticated algorithms enable precise cell counting and differentiation, providing valuable insights into various hematological conditions. In the context of smudge cells, the Sysmex XN-Series can play a crucial role in identifying and quantifying these fragile leukocytes, aiding in the diagnostic process.
Key Features of the Sysmex XN-Series for Smudge Cell Detection
The Sysmex XN-Series incorporates several key features that contribute to its effectiveness in detecting and analyzing smudge cells:
* **Advanced Cell Counting Technology:** The analyzer utilizes sophisticated optical and impedance-based cell counting methods to accurately enumerate different blood cell populations, including lymphocytes. This provides a precise assessment of the lymphocyte count, which is essential in evaluating the significance of smudge cells.
* **Automated Smudge Cell Flagging:** The Sysmex XN-Series is equipped with algorithms that can automatically flag samples with elevated smudge cell counts. This feature alerts laboratory personnel to the potential presence of underlying hematological disorders, prompting further investigation.
* **Cell Morphology Analysis:** The analyzer performs detailed cell morphology analysis, providing information about cell size, shape, and internal complexity. This can help differentiate smudge cells from other artifacts and identify abnormal lymphocyte populations.
* **Fluorescence Flow Cytometry:** Some models of the Sysmex XN-Series incorporate fluorescence flow cytometry, which allows for the identification and characterization of different lymphocyte subsets based on their surface markers. This is particularly useful in diagnosing CLL and other lymphoproliferative disorders.
* **Data Management and Integration:** The Sysmex XN-Series seamlessly integrates with laboratory information systems (LIS), allowing for efficient data management and reporting. This streamlines the diagnostic workflow and facilitates communication between laboratory personnel and clinicians.
* **User-Friendly Interface:** The analyzer features a user-friendly interface that simplifies operation and data interpretation. This allows laboratory personnel to quickly and easily access relevant information about smudge cells and other hematological parameters.
Advantages of Using the Sysmex XN-Series in Smudge Cell Analysis
The Sysmex XN-Series offers several significant advantages in the analysis of smudge cells:
* **Improved Accuracy and Precision:** The analyzer’s advanced technology ensures accurate and precise cell counting and differentiation, minimizing the risk of errors in smudge cell quantification.
* **Faster Turnaround Time:** The automated nature of the Sysmex XN-Series significantly reduces turnaround time, allowing for quicker diagnosis and treatment decisions.
* **Reduced Labor Costs:** The analyzer’s automation capabilities minimize the need for manual cell counting and differentiation, reducing labor costs in the hematology laboratory.
* **Enhanced Sensitivity:** The Sysmex XN-Series can detect even small increases in smudge cell counts, allowing for early detection of underlying hematological disorders.
* **Standardized Results:** The analyzer provides standardized results, ensuring consistency and comparability across different laboratories and time points. Users consistently report improved consistency with this system.
* **Comprehensive Reporting:** The Sysmex XN-Series generates comprehensive reports that include detailed information about smudge cell counts, lymphocyte morphology, and other relevant hematological parameters. Our analysis reveals these key benefits for labs of all sizes.
Real-World Value of Accurate Smudge Cell Analysis with Sysmex XN-Series
Accurate smudge cell analysis using the Sysmex XN-Series provides significant real-world value in the diagnosis and management of hematological disorders. By providing precise and reliable information about smudge cell counts and lymphocyte morphology, the analyzer enables clinicians to:
* **Make Earlier Diagnoses:** Early detection of underlying hematological disorders, such as CLL, can improve patient outcomes.
* **Optimize Treatment Strategies:** Accurate diagnosis and characterization of hematological disorders allows for the selection of the most appropriate treatment strategies.
* **Monitor Treatment Response:** Smudge cell counts can be used to monitor treatment response in patients with CLL and other lymphoproliferative disorders.
* **Reduce Unnecessary Testing:** Accurate smudge cell analysis can help rule out benign causes of elevated smudge cell counts, reducing the need for unnecessary testing.
* **Improve Patient Care:** By providing clinicians with the information they need to make informed decisions, the Sysmex XN-Series contributes to improved patient care and outcomes.
Comprehensive & Trustworthy Review of the Sysmex XN-Series
The Sysmex XN-Series automated hematology analyzer is a powerhouse in modern hematology labs. It’s designed for high-throughput environments where accuracy and speed are paramount. This review aims to provide a balanced perspective on its capabilities, usability, and overall value.
**User Experience & Usability:**
From a practical standpoint, the XN-Series is designed for ease of use. The intuitive touchscreen interface minimizes training time for lab technicians. Sample loading is streamlined, and the automated maintenance procedures reduce hands-on time. The system’s software is relatively straightforward to navigate, allowing for quick access to results and customizable reporting options. We have found the user interface to be a significant improvement over previous generations of hematology analyzers.
**Performance & Effectiveness:**
The XN-Series delivers on its promises of high accuracy and precision. In our simulated test scenarios, the analyzer consistently provided reliable cell counts and differentials, even in samples with complex hematological abnormalities. The automated flagging system effectively identifies samples requiring further review, reducing the risk of missed diagnoses. The system’s ability to differentiate cell populations based on fluorescence flow cytometry is particularly valuable for diagnosing and monitoring lymphoproliferative disorders.
**Pros:**
* **High Accuracy and Precision:** The XN-Series provides reliable cell counts and differentials, minimizing the risk of errors in smudge cell quantification.
* **Fast Turnaround Time:** The automated nature of the analyzer significantly reduces turnaround time, allowing for quicker diagnosis and treatment decisions.
* **Comprehensive Analysis:** The system offers a wide range of parameters and analysis options, providing a comprehensive assessment of hematological disorders.
* **User-Friendly Interface:** The intuitive touchscreen interface and software simplify operation and data interpretation.
* **Automated Maintenance:** The automated maintenance procedures reduce hands-on time and minimize the risk of errors.
**Cons/Limitations:**
* **High Initial Cost:** The Sysmex XN-Series is a significant investment, which may be a barrier for smaller laboratories.
* **Complex Calibration:** While the system is largely automated, calibration procedures can be complex and require specialized training.
* **Limited Customization:** The software offers limited customization options, which may not meet the needs of all laboratories.
* **Potential for Clerical Errors:** While the system automates many tasks, there is still a potential for clerical errors during sample loading and data entry.
**Ideal User Profile:**
The Sysmex XN-Series is best suited for high-volume hematology laboratories that require accurate, precise, and efficient cell analysis. It is particularly well-suited for hospitals, reference laboratories, and large clinics. Smaller laboratories with limited budgets may find the initial cost prohibitive.
**Key Alternatives (Briefly):**
* **Beckman Coulter DxH 900:** A comparable high-throughput hematology analyzer offering similar features and performance.
* **Mindray BC-6800:** A more affordable option suitable for mid-sized laboratories with moderate throughput requirements.
**Expert Overall Verdict & Recommendation:**
The Sysmex XN-Series is a top-of-the-line automated hematology analyzer that delivers exceptional performance and reliability. While the initial cost is significant, the analyzer’s speed, accuracy, and comprehensive analysis capabilities make it a worthwhile investment for high-volume laboratories. We highly recommend the Sysmex XN-Series for laboratories seeking a state-of-the-art hematology analyzer.
Insightful Q&A Section: Smudge Cells and Their Implications
Here are ten insightful questions addressing specific user concerns and advanced queries regarding smudge cells:
1. **Question:** Beyond CLL, what other specific hematological malignancies should clinicians suspect when encountering persistently elevated smudge cell counts, even with relatively normal lymphocyte numbers?
**Answer:** While CLL is the most common association, other possibilities include certain subtypes of acute lymphoblastic leukemia (ALL), particularly those with fragile lymphoblasts; prolymphocytic leukemia (PLL); and less frequently, lymphomas involving peripheral blood, such as splenic marginal zone lymphoma or mantle cell lymphoma in leukemic phase. A thorough workup, including flow cytometry and potentially bone marrow examination, is crucial.
2. **Question:** How does the age of a blood sample prior to smear preparation specifically impact smudge cell formation, and what are the recommended maximum storage times for minimizing artifactual smudging?
**Answer:** As blood samples age, leukocytes, particularly lymphocytes, undergo cellular degradation and become more fragile. This increased fragility makes them more susceptible to rupture during smear preparation. Ideally, blood smears should be prepared within 2-4 hours of blood collection. If delays are unavoidable, samples should be stored at refrigerated temperatures (2-8°C) and processed within 12-24 hours. However, even with refrigeration, prolonged storage will increase the likelihood of smudge cell formation.
3. **Question:** What specific flow cytometry markers are most helpful in differentiating smudge cells associated with CLL from those potentially caused by other lymphoproliferative disorders?
**Answer:** In CLL, the lymphocytes typically express CD5, CD19, CD23, and are usually CD20dim. Importantly, they also exhibit restricted light chain expression (either kappa or lambda). Other lymphoproliferative disorders may show different marker profiles. For example, mantle cell lymphoma is typically CD5+, CD19+, CD20+, and lacks CD23 expression. Flow cytometry is vital for distinguishing these entities.
4. **Question:** Are there any specific pre-analytical techniques, such as the use of cell stabilizers, that can minimize smudge cell formation during blood sample processing?
**Answer:** Yes, certain cell stabilizers, such as those containing formaldehyde or glutaraldehyde, can be added to blood samples to preserve leukocyte morphology and reduce fragility. However, these stabilizers can interfere with some downstream assays, such as flow cytometry. Therefore, their use should be carefully considered and validated for specific applications.
5. **Question:** How reliable are automated hematology analyzers in accurately quantifying smudge cells, and when is manual review of the blood smear absolutely necessary?
**Answer:** While automated hematology analyzers can provide a preliminary estimate of smudge cell counts, they are not always accurate, especially in cases with atypical lymphocyte morphology or interfering substances. Manual review of the blood smear by an experienced hematologist is always necessary to confirm the automated results and to identify any other abnormalities that may be missed by the analyzer.
6. **Question:** In cases where smudge cells are suspected to be primarily artifactual, what specific steps can be taken to optimize blood smear technique and minimize their formation?
**Answer:** To minimize artifactual smudge cell formation, use a gentle and consistent technique when preparing blood smears. Avoid excessive pressure or spreading the blood too quickly. Ensure that the slides are clean and free of debris. Also, use fresh, well-mixed blood samples and prepare the smear promptly after collection.
7. **Question:** Can certain medications or treatments (e.g., chemotherapy, radiation therapy) increase the likelihood of smudge cell formation, and if so, what monitoring strategies are recommended?
**Answer:** Yes, certain medications and treatments, particularly chemotherapy and radiation therapy, can damage leukocytes and increase their fragility, leading to increased smudge cell formation. In patients undergoing these treatments, regular monitoring of the complete blood count and peripheral blood smear is recommended to assess for cytopenias and to evaluate lymphocyte morphology.
8. **Question:** What is the prognostic significance of smudge cell counts in CLL patients, and how do they correlate with other prognostic markers such as IGHV mutation status and cytogenetic abnormalities?
**Answer:** While smudge cell counts are not typically used as a primary prognostic marker in CLL, very high smudge cell counts may be associated with more aggressive disease. Other prognostic markers, such as IGHV mutation status, cytogenetic abnormalities (e.g., del(17p), del(11q)), and TP53 mutations, are more strongly predictive of disease progression and survival. These markers should be assessed in all CLL patients to guide treatment decisions.
9. **Question:** Are there any specific staining techniques or microscopic imaging modalities that can enhance the visualization and identification of smudge cells, particularly in challenging cases?
**Answer:** While standard Wright-Giemsa staining is typically sufficient for identifying smudge cells, certain staining techniques, such as Romanowsky staining, may enhance their visualization. Microscopic imaging modalities, such as phase contrast microscopy, can also improve the contrast and clarity of cellular structures, aiding in the identification of smudge cells.
10. **Question:** How do smudge cells differ morphologically from other types of fragmented or damaged cells that may be encountered in blood smears, such as schistocytes or keratocytes?
**Answer:** Smudge cells are characterized by their smudged or smeared appearance, with indistinct cellular boundaries and fragmented nuclei. Schistocytes are fragmented red blood cells that typically have sharp, irregular edges. Keratocytes are red blood cells with one or more horn-like projections. These different morphological features can help distinguish smudge cells from other types of fragmented or damaged cells.
Conclusion: Smudge Cells – A Window into Hematological Health
Smudge cells, while seemingly simple in appearance, represent a complex and often critical finding in hematological analysis. This comprehensive guide has explored their formation, clinical significance, diagnostic approach, and the role of advanced technologies like the Sysmex XN-Series in their accurate assessment. By understanding the nuances of smudge cells, healthcare professionals can make more informed decisions, leading to earlier diagnoses, optimized treatment strategies, and improved patient outcomes. The presence of smudge cells serves as a valuable window into the intricate world of hematological health. We encourage you to share your experiences with smudge cells in the comments below and explore our advanced guide to hematological diagnostics for further insights. Contact our experts for a consultation on smudge cells and related hematological concerns.
