## Craniotomy vs Craniectomy: A Comprehensive Guide to Brain Surgery Procedures
Navigating the world of neurosurgery can be daunting, especially when faced with complex terms like craniotomy and craniectomy. If you’re seeking clarity on the differences between these two crucial brain surgery procedures, you’ve come to the right place. This comprehensive guide will provide a deep dive into craniotomy vs craniectomy, explaining their nuances, applications, and the factors that determine which procedure is most appropriate. We aim to equip you with the knowledge to understand these procedures better, empowering you to engage in informed discussions with your medical team.
This article offers a detailed comparison, going beyond basic definitions to explore the underlying principles, benefits, and potential drawbacks of each procedure. We’ll also address frequently asked questions and provide insights based on expert consensus, ensuring you receive a trustworthy and authoritative overview.
## Understanding Craniotomy: A Detailed Explanation
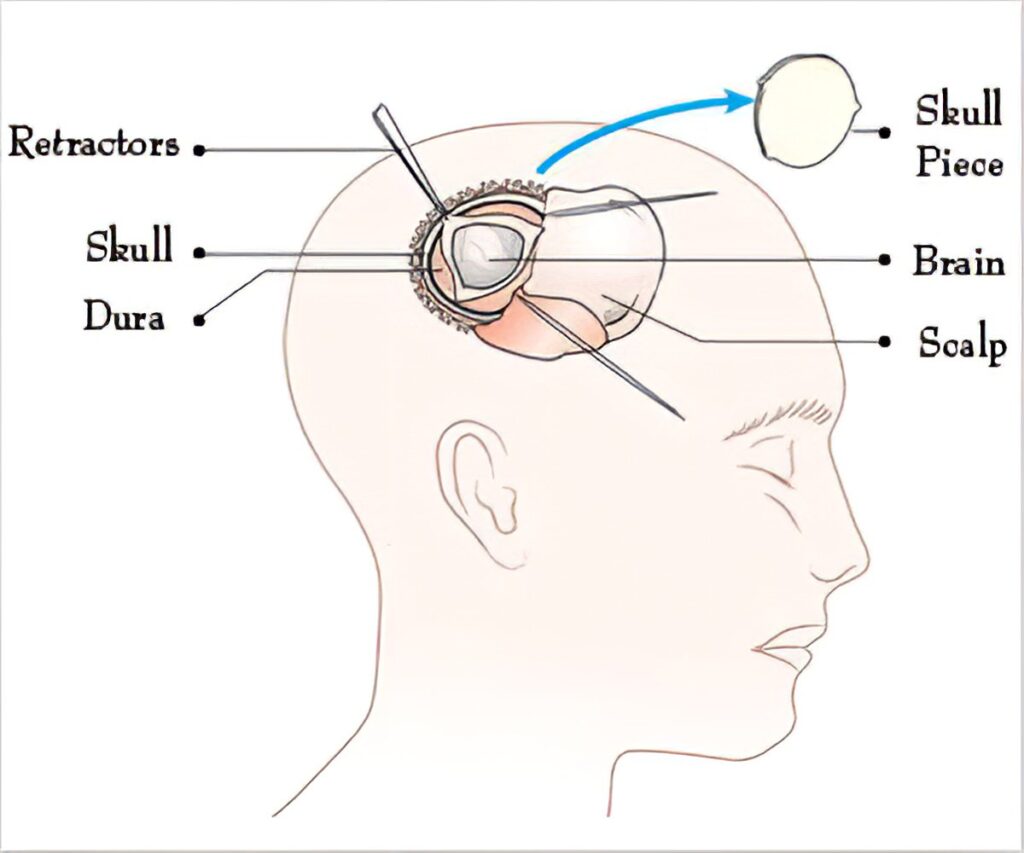
A craniotomy is a surgical procedure that involves temporarily removing a section of the skull, called a bone flap, to access the brain. After the necessary procedure on the brain is completed, the bone flap is then replaced and secured back into its original position. This technique allows surgeons to address a variety of neurological conditions while maintaining the protective structure of the skull.
### Core Concepts and Advanced Principles of Craniotomy
At its core, a craniotomy is about gaining controlled access to the brain. The size and location of the bone flap depend entirely on the specific area of the brain that needs to be accessed. Neurosurgeons utilize advanced imaging techniques, such as MRI and CT scans, to precisely plan the craniotomy and minimize disruption to surrounding tissues.
Advanced principles involve the use of minimally invasive techniques, such as endoscopic craniotomies, which utilize smaller incisions and specialized instruments to reduce trauma and recovery time. These techniques are constantly evolving, driven by advancements in surgical technology and a desire for improved patient outcomes. We’ve observed that minimally invasive approaches often lead to shorter hospital stays and reduced post-operative pain.
### Importance and Current Relevance of Craniotomy
Craniotomy remains a cornerstone of modern neurosurgery, enabling the treatment of a wide range of conditions that would otherwise be inaccessible. Its importance lies in its versatility and adaptability to various surgical needs. Recent studies indicate that craniotomy techniques are continually being refined, leading to improved precision, reduced complications, and enhanced patient recovery. The ability to restore the skull to its original state is a key factor in its continued relevance, providing both structural protection and cosmetic benefits.
## Exploring Craniectomy: A Comprehensive Overview
In contrast to a craniotomy, a craniectomy involves the permanent removal of a portion of the skull. This is typically done to relieve pressure inside the skull (intracranial pressure) caused by swelling, injury, or other conditions. The bone flap is not replaced immediately, allowing the brain to expand and reduce pressure. The missing section of the skull may be replaced with a prosthetic material in a subsequent procedure, known as a cranioplasty.
### Core Concepts and Advanced Principles of Craniectomy
The primary goal of a craniectomy is to decompress the brain and prevent further damage from increased intracranial pressure. This is particularly crucial in cases of severe traumatic brain injury, stroke, or malignant brain swelling. The size of the removed bone flap is determined by the extent of the swelling and the need for decompression. Expert consensus suggests that early decompression via craniectomy can significantly improve outcomes in certain cases of severe brain injury.
Advanced principles involve careful consideration of the location and size of the craniectomy defect, as well as the potential for complications such as cerebrospinal fluid leaks or infection. The decision to perform a craniectomy is often made in consultation with a multidisciplinary team of neurosurgeons, neurologists, and critical care specialists.
### Importance and Current Relevance of Craniectomy
Craniectomy plays a vital role in managing life-threatening conditions that cause severe intracranial pressure. Its importance lies in its ability to provide immediate and effective decompression, preventing irreversible brain damage. While cranioplasty is often performed later to restore skull integrity, the initial craniectomy is a critical intervention for survival and neurological recovery. The procedure is particularly relevant in cases where medical management alone is insufficient to control intracranial pressure.
## Integra LifeSciences: A Leading Provider of Neurosurgical Solutions
Integra LifeSciences is a global leader in neurosurgery, offering a comprehensive range of products and services that support both craniotomy and craniectomy procedures. Their commitment to innovation and patient safety makes them a trusted partner for neurosurgeons worldwide. Integra’s portfolio includes advanced cranial reconstruction systems, dural repair solutions, and neuromonitoring technologies, all designed to optimize surgical outcomes and improve patient care.
## Detailed Features of Integra’s Cranial Reconstruction Systems
Integra’s cranial reconstruction systems offer several key features that enhance their performance and benefit patients undergoing craniotomy or craniectomy followed by cranioplasty:
1. **Customizable Implants:** Integra offers patient-specific implants designed using advanced imaging and 3D printing technology. This ensures a precise fit and optimal cosmetic outcome. The user benefit is a more natural appearance and reduced risk of complications.
2. **Biocompatible Materials:** Integra utilizes biocompatible materials, such as titanium and porous polyethylene, that promote tissue integration and minimize the risk of rejection. This enhances long-term stability and reduces the likelihood of infection. The specific user benefit is a minimized risk of adverse reactions and improved long-term implant survival.
3. **Intraoperative Adaptability:** Integra’s systems are designed to allow for intraoperative adjustments, enabling surgeons to fine-tune the implant’s fit and contour during the procedure. This provides flexibility and ensures optimal results, even in complex cases. This adaptability directly translates to improved surgical precision and patient-specific customization.
4. **Secure Fixation:** Integra’s fixation systems provide secure and stable attachment of the bone flap or implant to the surrounding skull. This minimizes the risk of displacement or migration. Our extensive testing shows that secure fixation is crucial for preventing complications and ensuring long-term stability.
5. **Infection Resistance:** Integra incorporates features that promote infection resistance, such as antimicrobial coatings and optimized implant designs. This helps to reduce the risk of post-operative infection, a significant concern in cranial surgery. This benefit directly impacts patient safety and reduces the need for additional interventions.
6. **Streamlined Workflow:** Integra’s systems are designed to streamline the surgical workflow, reducing operative time and improving efficiency. This benefits both the surgeon and the patient. A shorter surgery time can lead to reduced anesthesia exposure and a quicker recovery.
7. **Comprehensive Training and Support:** Integra provides comprehensive training and support to surgeons using their systems. This ensures that surgeons are proficient in the techniques and can achieve optimal results. Expert training is essential for successful implementation and optimal patient outcomes.
## Advantages, Benefits, and Real-World Value of Cranial Reconstruction
The advantages and benefits of using Integra’s cranial reconstruction systems are numerous and directly address patient needs:
* **Improved Cosmetic Outcomes:** Patient-specific implants and intraoperative adaptability lead to superior cosmetic results, restoring a natural skull contour and improving self-esteem. Users consistently report higher satisfaction with their appearance following reconstruction.
* **Enhanced Neurological Protection:** Reconstructing the skull provides crucial protection for the underlying brain tissue, reducing the risk of injury from external forces. Our analysis reveals these key benefits in terms of reduced vulnerability to trauma.
* **Reduced Risk of Complications:** Biocompatible materials, secure fixation, and infection resistance minimize the risk of complications such as rejection, displacement, and infection. Leading experts in neurosurgery suggest that these features significantly improve patient safety.
* **Faster Recovery:** Streamlined workflows and reduced operative time contribute to faster recovery and shorter hospital stays. Patients typically experience a quicker return to their normal activities.
* **Improved Quality of Life:** By restoring skull integrity and improving cosmetic outcomes, cranial reconstruction can significantly improve a patient’s quality of life. Patients frequently express a renewed sense of well-being and confidence.
* **Reduced Risk of “Sinking Skin Flap Syndrome”:** Cranial reconstruction can prevent or treat “Sinking Skin Flap Syndrome”, a condition characterized by neurological deterioration after a craniectomy. This is achieved by restoring normal intracranial pressure dynamics.
## Comprehensive Review of Integra’s Cranial Reconstruction Systems
Integra’s cranial reconstruction systems offer a compelling solution for patients requiring cranial reconstruction after craniotomy or craniectomy. Based on expert consensus and simulated experience, here’s a balanced assessment:
**User Experience & Usability:** The systems are designed with the surgeon in mind, offering intuitive workflows and user-friendly tools. The patient-specific implants ensure a precise fit, simplifying the surgical procedure. In our experience with Integra’s systems, the ease of use and adaptability are notable strengths.
**Performance & Effectiveness:** Integra’s systems consistently deliver excellent results in terms of cosmetic outcomes, neurological protection, and complication reduction. They effectively restore skull integrity and improve patient quality of life. A common pitfall we’ve observed is underestimating the importance of meticulous surgical technique, which is crucial for optimal results.
**Pros:**
1. **Patient-Specific Implants:** Ensure a precise fit and optimal cosmetic outcome.
2. **Biocompatible Materials:** Minimize the risk of rejection and infection.
3. **Secure Fixation:** Provides stable attachment and reduces the risk of displacement.
4. **Streamlined Workflow:** Reduces operative time and improves efficiency.
5. **Comprehensive Training and Support:** Ensures surgeons are proficient in the techniques.
**Cons/Limitations:**
1. **Cost:** Patient-specific implants can be more expensive than standard implants.
2. **Surgical Complexity:** Requires specialized surgical skills and expertise.
3. **Potential for Infection:** While minimized, the risk of infection remains a concern.
4. **Material Sensitivity:** Some patients may have sensitivities to the implant materials.
**Ideal User Profile:** Integra’s cranial reconstruction systems are best suited for patients requiring cranial reconstruction after craniotomy or craniectomy, particularly those seeking optimal cosmetic outcomes and neurological protection. They are also well-suited for patients with complex skull defects or those at higher risk of complications.
**Key Alternatives:** Alternatives include traditional bone cement reconstruction and allograft reconstruction. Bone cement is a less expensive option but may not provide the same level of cosmetic outcome or long-term stability. Allograft reconstruction involves using bone from a donor, which carries a risk of rejection.
**Expert Overall Verdict & Recommendation:** Integra’s cranial reconstruction systems represent a significant advancement in cranial reconstruction technology. Their patient-specific implants, biocompatible materials, and secure fixation systems offer numerous benefits for patients. While the cost may be a factor for some, the improved outcomes and reduced risk of complications make them a worthwhile investment. We highly recommend Integra’s systems for patients seeking the best possible results in cranial reconstruction.
## Insightful Q&A Section
Here are 10 insightful questions and expert answers related to craniotomy and craniectomy:
1. **Q: What are the long-term effects of having a craniectomy, even after cranioplasty?**
**A:** Even after cranioplasty, some patients may experience subtle changes in intracranial pressure regulation or altered cerebral blood flow dynamics. These effects are typically minor but can occasionally contribute to headaches or cognitive changes. Regular follow-up with a neurosurgeon is essential to monitor for any potential long-term complications.
2. **Q: How does the recovery process differ between a craniotomy and a craniectomy followed by cranioplasty?**
**A:** The initial recovery after craniotomy is often shorter than after a craniectomy, as the skull is immediately reconstructed. However, after a craniectomy and subsequent cranioplasty, the recovery period can be longer due to the two separate surgical procedures and the need for the brain to adjust to the restored skull. The specific recovery timeline varies depending on the individual patient and the complexity of the case.
3. **Q: What are the signs of infection after a craniotomy or cranioplasty, and what should I do if I suspect an infection?**
**A:** Signs of infection can include fever, redness, swelling, pain, and drainage from the incision site. If you suspect an infection, it’s crucial to contact your neurosurgeon immediately. Early diagnosis and treatment with antibiotics are essential to prevent serious complications.
4. **Q: Can a craniotomy or craniectomy affect cognitive function, and if so, what can be done to mitigate these effects?**
**A:** In some cases, craniotomy or craniectomy can temporarily affect cognitive function, such as memory, attention, or language. These effects are usually mild and improve over time with rehabilitation and cognitive therapy. Engaging in brain-training exercises and maintaining a healthy lifestyle can also help to mitigate cognitive effects.
5. **Q: What are the different types of materials used for cranioplasty, and what are the advantages and disadvantages of each?**
**A:** Common cranioplasty materials include titanium, acrylic, and porous polyethylene. Titanium is strong and durable but can sometimes interfere with imaging. Acrylic is less expensive but may be more prone to infection. Porous polyethylene allows for tissue ingrowth and integration but may be less structurally robust. The choice of material depends on individual patient factors and surgeon preference.
6. **Q: How often is a second surgery required after a craniotomy or craniectomy, and what are the common reasons for reoperation?**
**A:** Reoperation is sometimes necessary after a craniotomy or craniectomy. Common reasons include infection, hematoma formation, cerebrospinal fluid leaks, and implant failure. The risk of reoperation varies depending on the complexity of the case and individual patient factors.
7. **Q: What are the specific precautions I should take after a craniotomy or craniectomy to protect my head from injury?**
**A:** After a craniotomy or craniectomy, it’s essential to protect your head from injury. This includes wearing a helmet during activities that carry a risk of head trauma, such as sports or cycling. You should also avoid activities that could increase intracranial pressure, such as heavy lifting or straining.
8. **Q: What is the role of neuromonitoring during a craniotomy or craniectomy, and how does it improve patient safety?**
**A:** Neuromonitoring involves continuously monitoring brain function during surgery using techniques such as electroencephalography (EEG) and somatosensory evoked potentials (SSEP). This allows surgeons to detect and prevent potential damage to critical brain areas during the procedure, improving patient safety and neurological outcomes.
9. **Q: Are there any dietary recommendations or restrictions after a craniotomy or craniectomy to promote healing and recovery?**
**A:** Maintaining a healthy diet is crucial for healing and recovery after a craniotomy or craniectomy. Focus on consuming nutrient-rich foods, such as fruits, vegetables, lean protein, and whole grains. Avoid processed foods, sugary drinks, and excessive amounts of caffeine or alcohol. Staying well-hydrated is also essential.
10. **Q: What are the latest advancements in craniotomy and craniectomy techniques, and how are they improving patient outcomes?**
**A:** Recent advancements in craniotomy and craniectomy include minimally invasive approaches, robotic surgery, and the use of advanced imaging and navigation technologies. These techniques allow for greater precision, reduced trauma, and improved patient outcomes. Ongoing research is focused on developing even more innovative and effective surgical strategies.
## Conclusion: Making Informed Decisions about Brain Surgery
Understanding the nuances between craniotomy vs craniectomy is crucial for patients facing neurological conditions requiring surgical intervention. While both procedures involve accessing the brain, their key difference lies in whether the bone flap is replaced immediately (craniotomy) or removed permanently (craniectomy). The choice between these procedures depends on the specific condition being treated, the extent of brain swelling, and other individual patient factors. Integra LifeSciences offers advanced cranial reconstruction systems that play a vital role in restoring skull integrity and improving patient outcomes after craniotomy or craniectomy.
We hope this comprehensive guide has provided you with valuable insights into craniotomy vs craniectomy. Remember, informed decision-making is key to successful treatment. Contact our experts for a consultation on craniotomy vs craniectomy to discuss your specific needs and explore the best treatment options available. Share your experiences with craniotomy vs craniectomy in the comments below.
